AERD Risk Assessment Tool
This assessment tool helps you determine if your symptoms match Aspirin-Exacerbated Respiratory Disease (AERD), also known as Samter's Triad. AERD is a condition where asthma, chronic nasal polyps, and sensitivity to aspirin or NSAIDs occur together.
Based on research, having two or more of these symptoms increases the likelihood of AERD. This tool is not a diagnosis but can help you discuss your symptoms with a healthcare provider.
What Is Aspirin-Exacerbated Respiratory Disease?
Aspirin-Exacerbated Respiratory Disease is a chronic condition where asthma, chronic nasal polyps, and sensitivity to aspirin or NSAIDs occur together. It’s also known as Samter’s Triad or NSAID-ERD. Unlike typical allergies, this isn’t caused by an immune reaction to the drug itself. Instead, it’s a metabolic dysfunction in how your body handles inflammation.
People with AERD don’t suddenly become sensitive to aspirin. The condition develops over time, usually in adulthood between ages 20 and 50. It hits about 9% of all adults with asthma - and up to 30% of those who also have nasal polyps. The trigger isn’t the drug. It’s what happens inside your body when you take it.
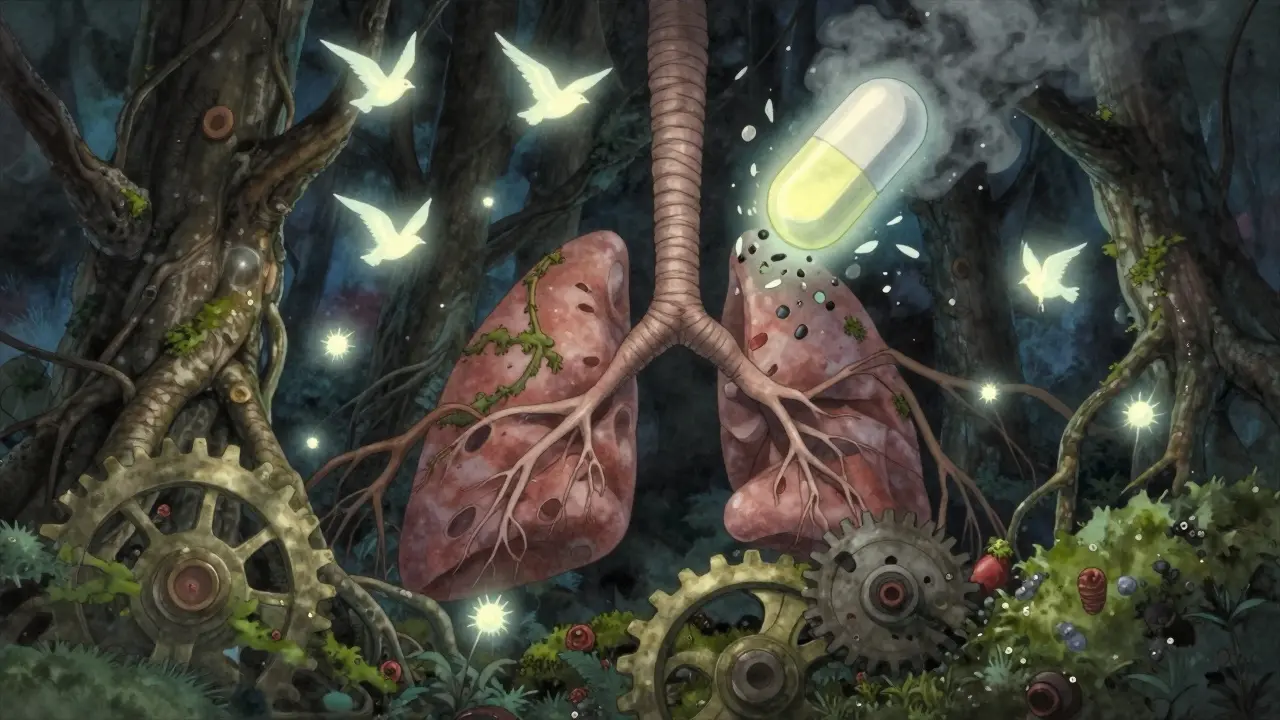
How AERD Changes Your Body’s Chemistry
When you take aspirin or NSAIDs like ibuprofen or naproxen, they block an enzyme called COX-1. For most people, that’s fine - it reduces pain and swelling. But in AERD, blocking COX-1 throws your body’s inflammatory system out of balance.
Your body starts producing too much of certain inflammatory chemicals called leukotrienes, especially leukotriene E4. At the same time, it makes less of prostaglandin E2, which normally keeps inflammation in check. This imbalance turns your airways into a storm zone. Your nose swells, your sinuses get clogged, and your lungs tighten up.
Studies show this triggers a strong Type 2 immune response - think high levels of IL-4, IL-13, and IL-5. These signals pull in eosinophils, a type of white blood cell that causes tissue damage. That’s why nasal polyps grow back so fast after surgery in AERD patients.
What Happens When You Take NSAIDs?
For someone with AERD, taking even a regular dose of ibuprofen can cause a reaction within 30 to 120 minutes. Symptoms aren’t mild. They’re intense and often scary.
- Severe nasal congestion - happens in 95% of reactions
- Frontal headache or sinus pressure - 88%
- Red, watery eyes - 76%
- Wheezing, chest tightness, coughing - 92%
Some people also get nausea, vomiting, stomach pain, flushing, or a rash. These reactions aren’t random. They’re predictable. And they’re not just about the nose or lungs. The whole respiratory system goes into overdrive.
What’s surprising to many? Alcohol can trigger the same reaction in about 75% of AERD patients. You don’t need to get drunk. Even one glass of wine or beer can cause congestion, coughing, or wheezing. This isn’t about the alcohol content - it’s about how it interacts with your inflamed airways.
Why AERD Is Worse Than Regular Asthma
AERD isn’t just asthma with a side of nasal polyps. It’s a more aggressive, harder-to-control version.
People with AERD have:
- Polyps that grow back faster - 70-100% recur within 18 months after surgery
- Worse asthma control - only 35% respond well to standard inhalers
- More ER visits - 2.3 times more than non-AERD asthma patients
- More hospital stays - 1.8 times more frequent
Standard asthma treatments like albuterol or inhaled steroids often don’t cut it. That’s because the inflammation driving AERD isn’t the same kind as in allergic asthma. It’s deeper, more systemic, and harder to quiet with typical meds.
Many patients end up needing multiple sinus surgeries. But removing polyps doesn’t fix the root problem. The inflammation keeps coming back. That’s why just avoiding NSAIDs isn’t enough - it doesn’t slow the disease.
The Long Road to Diagnosis
Most people with AERD wait years before getting the right diagnosis. On average, it takes 7 to 10 years.
Why? Because doctors don’t always connect the dots. A patient might see an allergist for asthma, an ENT for polyps, and a GP for headaches - but no one puts it all together. Reddit user PolypWarrior87 shared how it took 11 years and four specialists before someone finally linked their asthma attacks to Advil and their polyps.
There’s a pattern: adult-onset asthma + recurring nasal polyps + reaction to NSAIDs or alcohol. That’s the triad. If you have two of those, you should be tested. If you have all three, it’s almost certainly AERD.
Yet, many primary care doctors and even some allergists miss the alcohol trigger. One study found that 75% of AERD patients react to alcohol - but only a fraction of clinicians ask about it.
The Only Treatment That Actually Works
There’s one treatment that changes the course of AERD: aspirin desensitization.
This isn’t a cure. But it’s the closest thing we have. In a controlled hospital setting, patients are given gradually increasing doses of aspirin over two to three days. Once the body adjusts, they’re kept on a daily maintenance dose - usually 650 mg twice a day.
The results? 85% of patients see better asthma control. Sinus surgery needs drop by 60%. Polyp regrowth slows from every 6 months to every 2-3 years. One patient on the Samter’s Society forum, NoseFree99, said their polyps went from recurring every six months to every three years after desensitization.
It’s not risk-free. About 42% of patients have reactions during the process. That’s why it’s only done in specialized centers with emergency equipment on hand. But for those who complete it, the quality of life improvement is massive. A 2022 survey found 68% of patients reported significant gains.
What About Biologics and New Drugs?
Biologics like dupilumab (Dupixent) are now being used for AERD. It’s a shot that blocks IL-4 and IL-13 - two key players in the Type 2 inflammation that drives polyps and asthma.
Studies show it reduces polyp size by 50-60% and improves breathing. But it’s expensive - $38,500 a year - and only 38% of AERD patients have insurance coverage. It’s also not a replacement for aspirin desensitization. Many specialists use both together.
New drugs are coming. In June 2023, the FDA gave breakthrough status to MN-001 (lodadustat), a leukotriene inhibitor. Phase 2 trials showed a 70% drop in polyp recurrence. If it gets approved, it could be a game-changer for those who can’t tolerate daily aspirin.

Where to Get Help
There are only about 35 specialized AERD centers in the U.S. Most are tied to academic hospitals. Community clinics rarely offer desensitization - only 12% of allergy practices do.
If you suspect you have AERD, start by asking your doctor for a referral to an allergist-immunologist who specializes in respiratory diseases. Don’t settle for general care. This condition needs experts.
Support groups like the Samter’s Society (samterssociety.org) offer free resources: 127 articles, 28 patient videos, and a community of over 2,300 people who’ve been through it. Their patient portal has a 4.5/5 rating for clarity and usefulness.
Specialized centers also offer 24/7 nurse hotlines. One patient told me they got a call back in under two hours when they panicked after a reaction. At a regular clinic? They waited three days.
What You Can Do Today
If you have asthma and nasal polyps, and you’ve ever had a reaction to ibuprofen, aspirin, or alcohol - don’t wait. Write down your symptoms: when they happened, what you took, how long it took to react.
Ask your doctor: Could this be AERD? If they say no or don’t know, ask for a referral to an AERD specialist. You don’t need to suffer for another decade.
Don’t avoid NSAIDs just because you’re scared. Avoidance doesn’t stop the disease. It just leaves you stuck with worsening symptoms and repeated surgeries.
Desensitization is hard. It takes time. But for most people, it’s the only way to take back control of their breathing, their sense of smell, and their life.
Why This Matters
AERD affects 1.2 million Americans. It costs the system $1.8 billion a year in surgeries, ER visits, and lost workdays. But the human cost is higher.
People lose their sense of smell. They can’t enjoy food. They can’t sleep because their nose is blocked. They miss work, cancel plans, and live in fear of a simple painkiller.
And it’s worse for Black and Hispanic patients - they wait 3.2 years longer for diagnosis. That’s not just a gap. It’s a failure of the system.
This isn’t rare. It’s underdiagnosed. And it’s treatable.
14 Comments
Write a comment
More Articles

Contamination Issues in Generic Drugs: Recent Cases and How to Prevent Them
Recent contamination cases in generic drugs-including NDMA in valsartan and benzene in Mucinex-reveal serious safety gaps. Learn what’s behind the recalls, who’s affected, and how to protect yourself.



Abby Polhill
December 25, 2025 AT 01:58So AERD isn't just an allergy-it's a metabolic cascade gone rogue. The COX-1 inhibition leading to leukotriene surges? That’s the core. And the fact that alcohol triggers it via the same pathway? Mind blown. This isn't 'can't have ibuprofen'-it's 'your entire Type 2 immune axis is dysregulated.'
Biologics like dupilumab make sense mechanistically-blocking IL-4/IL-13 hits the eosinophilic firestorm. But the cost? Criminal. Insurance denials are the real epidemic here.
And yes, the 7–10 year diagnostic delay? That’s systemic failure. Primary care docs still think 'asthma + polyps' = allergic rhinitis. They don't connect the dots to NSAID sensitivity. We need mandatory screening protocols for adult-onset asthma with polyps. Period.