DOAC Dosing Calculator for Renal Impairment
Dosing Calculator
Results will appear here
Enter patient details to see the calculated CrCl and appropriate DOAC dosing recommendations.
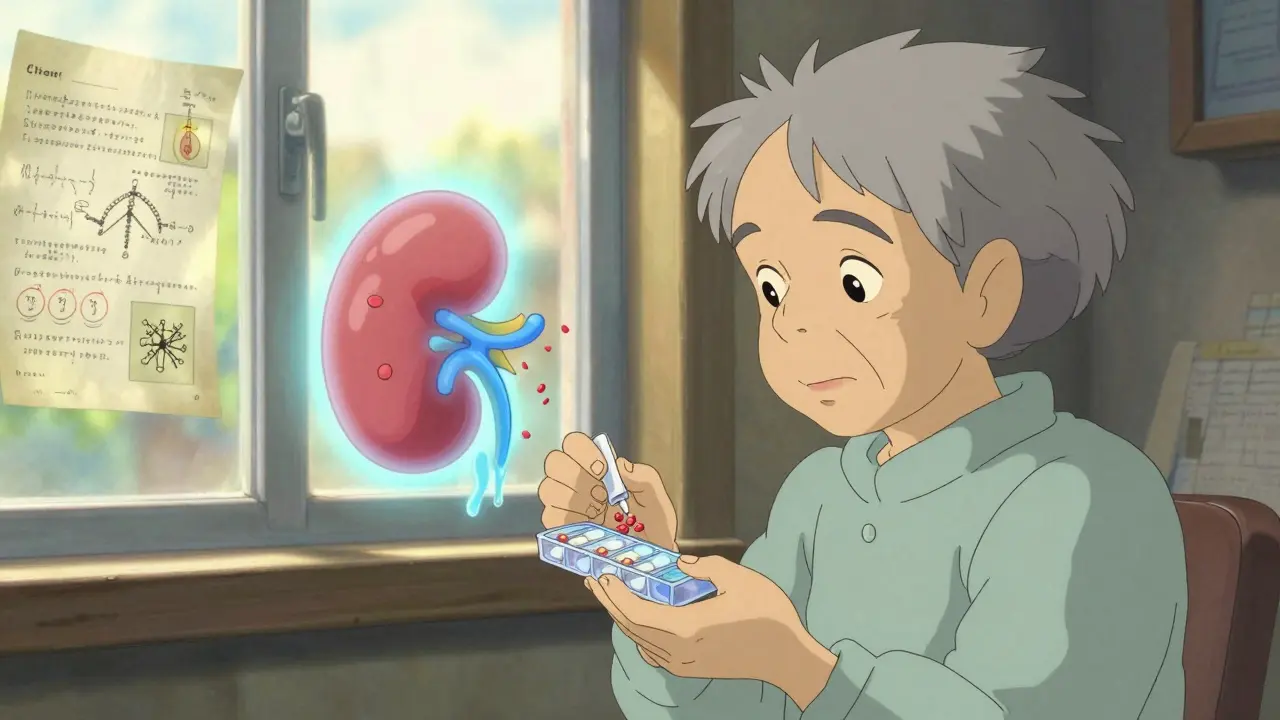
When your kidneys aren't working well, taking a blood thinner like apixaban or rivaroxaban can be risky-if you don’t adjust the dose. Direct Oral Anticoagulants (DOACs) are meant to be simpler than warfarin: no regular blood tests, fewer food interactions, and more predictable effects. But when kidney function drops, that predictability disappears. Too much drug builds up in your system and increases bleeding risk. Too little and you’re unprotected against strokes or clots. The difference between safety and danger often comes down to one thing: correct dosing based on real kidney function.
Why Renal Impairment Changes Everything
DOACs don’t just pass through your body-they’re cleared by your kidneys. Apixaban, rivaroxaban, dabigatran, and edoxaban all rely on the kidneys to remove them. When your kidneys slow down, these drugs stick around longer. That might sound harmless, but it’s not. In someone with severe kidney disease, a standard dose can become toxic. A 2022 study in JAMA Internal Medicine found that nearly 4 out of 10 prescriptions for DOACs in patients with chronic kidney disease were dosed incorrectly. Many of those errors led to serious bleeding or hospitalization. The problem isn’t just the drug. It’s how we measure kidney function. Most doctors use eGFR-the estimated glomerular filtration rate-from routine blood tests. But for DOACs, that number doesn’t cut it. The FDA and major guidelines require the Cockcroft-Gault formula to calculate creatinine clearance (CrCl). This formula factors in age, weight, sex, and serum creatinine. It’s older than most of us, but it’s still the gold standard. Using eGFR instead? You could be underdosing or overdosing without even knowing it.How Each DOAC Should Be Dosed in Kidney Disease
There’s no one-size-fits-all answer. Each DOAC has its own rules. Here’s what you need to know:- Apixaban: Standard dose is 5 mg twice daily. But if you’re 80 or older, weigh 60 kg or less, and have a creatinine level of 133 μmol/L or higher, drop to 2.5 mg twice daily. This applies even if your CrCl is above 30 mL/min. For CrCl between 15 and 29 mL/min, use 2.5 mg twice daily. Never use it if CrCl is below 15 mL/min.
- Rivaroxaban: Avoid entirely if CrCl is below 15 mL/min. For CrCl between 15 and 49 mL/min, reduce to 15 mg once daily. Do not use for stroke prevention in atrial fibrillation if you’re on dialysis.
- Dabigatran: Reduce to 75 mg twice daily if CrCl is 15-30 mL/min. Not recommended below 15 mL/min. It’s the most heavily cleared by kidneys-so it’s the riskiest in advanced disease.
- Edoxaban: Reduce to 30 mg once daily if CrCl is 15-50 mL/min. Contraindicated below 15 mL/min.
Here’s the key point: apixaban is the most forgiving. It’s the only DOAC with enough data to support its use-even in patients on hemodialysis. A 2020 study in the Journal of the American Heart Association showed apixaban had lower bleeding rates than warfarin in end-stage kidney disease. That’s why nephrologists in Sydney and Toronto are increasingly choosing apixaban over warfarin for dialysis patients.
The Apixaban Advantage in Advanced Kidney Disease
While other DOACs are off-limits in severe kidney failure, apixaban has a quiet edge. About 20% of its clearance happens through the liver. That means even if your kidneys are failing, your body still has a backup way to get rid of it. That’s not true for dabigatran or edoxaban-over 80% leaves through the kidneys. Dr. Sarah Kim, a nephrologist in Melbourne, tracked 127 dialysis patients on apixaban 2.5 mg twice daily over 18 months. Her major bleeding rate? Just 1.8%. In her previous warfarin group, it was 3.7%. That’s a 50% drop. She doesn’t call it a cure-but it’s a major improvement. But don’t assume apixaban is safe just because it’s used in dialysis. One case reported on a nephrology forum involved a 78-year-old man on standard-dose apixaban (5 mg twice daily) who suffered life-threatening gastrointestinal bleeding. He met two of the three criteria for dose reduction-he was over 80 and weighed 58 kg-but he was never switched. That’s the danger: assuming the drug is always safe, even when the rules say otherwise.Who Should Avoid DOACs Altogether?
There are clear red flags:- CrCl below 15 mL/min for all DOACs except apixaban (which is still used cautiously)
- Patients on hemodialysis who haven’t been studied in large trials-except for apixaban
- Those with uncontrolled high blood pressure or active bleeding
- People with a history of severe gastrointestinal bleeding or brain hemorrhage
Warfarin isn’t perfect-it needs frequent blood tests, interacts with food and other drugs, and still carries a high risk of bleeding in advanced kidney disease. But in patients with CrCl under 15 mL/min who aren’t candidates for apixaban, warfarin may still be the safest option. The American Heart Association still lists it as an option for end-stage kidney disease, even though DOACs are preferred in milder cases.
How to Get the Dose Right Every Time
Here’s a practical checklist:- Calculate CrCl using Cockcroft-Gault. Don’t rely on eGFR. Use this formula: (140 - age) × weight (kg) × (0.85 if female) / (72 × serum creatinine). Online calculators help, but always double-check.
- Check the three apixaban criteria: Age ≥80? Weight ≤60 kg? Creatinine ≥133 μmol/L? If two or more apply, use 2.5 mg twice daily-even if CrCl is normal.
- Recheck kidney function every 3-6 months. Kidney function can change fast, especially in older adults or those with heart failure or diabetes.
- Use a pharmacist’s help. Pharmacists are trained to catch dosing errors. In one hospital study, pharmacist-led reviews cut DOAC dosing mistakes by 60%.
- Don’t assume “low dose” means “safe”. Even reduced doses can be too high if kidney function declines suddenly.
Many doctors still miss the ABCs of apixaban. The mnemonic-Age, Body weight, Creatinine-is taught in residency programs for a reason. It’s simple, memorable, and prevents errors.

What’s Coming Next?
The RENAL-AF trial, expected to finish in 2025, is comparing apixaban to warfarin in patients with severe kidney disease. Early data from small studies suggest apixaban is safer and just as effective. If the results hold, we may see official guidelines change to make apixaban the first choice for all stages of kidney disease. Meanwhile, virtual anticoagulation clinics are popping up across Australia and the U.S. These online services monitor kidney function, check medication lists, and alert doctors when doses need adjusting. One study showed they reduced bleeding events by over 20%. That’s not magic-it’s just better systems.Bottom Line: Do It Right, or Don’t Do It
DOACs are powerful tools. But in kidney disease, they’re like a scalpel without a handle. Use them without the right dose, and you risk cutting too deep-or not cutting deep enough. The data is clear: apixaban, when dosed properly, is the safest option for most people with kidney impairment. For those with end-stage disease, it’s often the only DOAC worth considering.Don’t let outdated habits or lazy calculations put your patient at risk. Always calculate CrCl. Always check the criteria. Always retest. Because in renal impairment, the right dose isn’t just a recommendation-it’s the line between life and death.
Can I use DOACs if I’m on dialysis?
Yes-but only apixaban, and only at a reduced dose of 2.5 mg twice daily. Rivaroxaban, dabigatran, and edoxaban are not recommended for patients on dialysis. Warfarin is still an option if apixaban isn’t suitable, but studies show apixaban has lower bleeding rates in this group.
Why can’t I just use eGFR to adjust my DOAC dose?
eGFR is useful for tracking general kidney health, but it doesn’t accurately reflect how fast your body clears DOACs. The Cockcroft-Gault formula, which includes weight and age, is the only method validated for DOAC dosing. Using eGFR can lead to underdosing or overdosing-and either one can be dangerous.
Is apixaban safe for elderly patients with low body weight?
Yes-but only if you reduce the dose. If you’re 80 or older, weigh 60 kg or less, and have elevated creatinine, you must take 2.5 mg twice daily, not the standard 5 mg. Many older patients are prescribed the full dose by mistake. That’s a common cause of bleeding in this group.
What happens if I miss a kidney function test?
Your DOAC dose could become unsafe. Kidney function can decline quickly, especially in people with diabetes, heart failure, or dehydration. Without regular CrCl checks, you might be taking too much drug. Guidelines recommend testing every 3-6 months for patients with CKD. If you’re over 75 or have other health issues, test every 3 months.
Can I switch from warfarin to a DOAC if I have kidney disease?
Yes-if your kidney function is above 30 mL/min, switching to apixaban or rivaroxaban is often safer than staying on warfarin. But if your CrCl is below 30, you need careful evaluation. Apixaban is the best choice in moderate to severe kidney disease. Never switch without recalculating CrCl and confirming the correct dose.
12 Comments
Write a comment
More Articles

Understanding the Link Between Idiopathic Orthostatic Hypotension and Chronic Pain
Explore how idiopathic orthostatic hypotension and chronic pain share autonomic dysfunction, learn diagnostic steps, and discover combined treatment strategies for better relief.


Mike Rengifo
December 19, 2025 AT 04:43Been using apixaban for AFib with CKD stage 3. Doc used eGFR and gave me 5mg twice. Ended up in the ER with a GI bleed. Turned out my CrCl was 22. Switched to 2.5mg and haven’t had a problem since. Always double-check the Cockcroft-Gault. Don’t trust the auto-calc in the EHR.