By 2025, the way healthcare providers think about their work has changed more in five years than it did in the previous two decades. It’s not just about new tools or bigger budgets. It’s a quiet but deep shift in healthcare provider attitudes-toward technology, patients, and even their own roles in the system.
Doctors Aren’t Just Diagnosing Anymore-They’re Interpreting Data
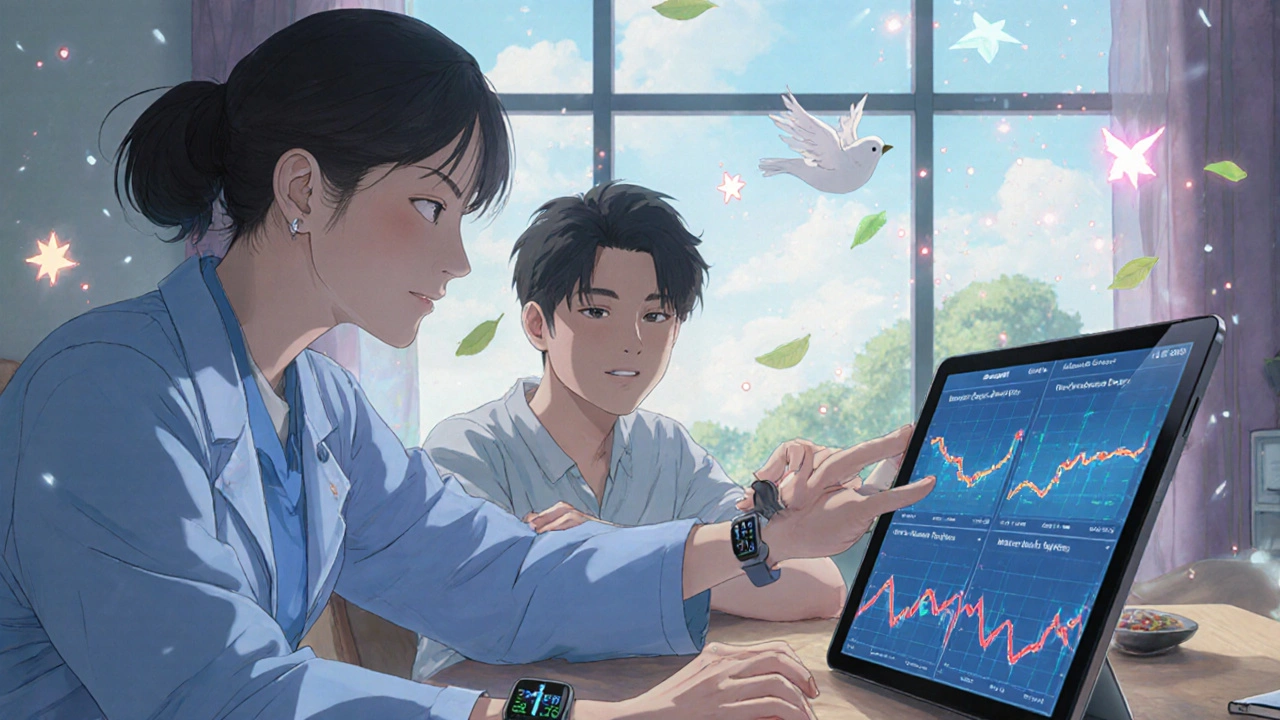
Five years ago, a patient walking into a clinic with a smartwatch reading their heart rate or sleep patterns might’ve been seen as overeager. Now, it’s expected. According to the NIH, patients arriving with their own health data-collected from wearables, apps, and home monitors-is the new normal. Providers aren’t just listening to symptoms anymore. They’re analyzing trends in glucose levels, oxygen saturation, and activity spikes over weeks or months. This changes everything. Instead of asking, "How have you been feeling?" providers now ask, "What did your device show last Tuesday?" That shift means doctors need new skills: not just medical knowledge, but data literacy. They’re learning to spot anomalies in consumer-generated data, understand what’s noise versus what’s a real signal, and explain it to patients who already think they know what’s wrong. Nature Digital Medicine confirmed in early 2025 that providers who once dismissed wearable data as unreliable now see it as essential for personalized care. One primary care physician in Melbourne told a researcher, "I used to doubt the numbers. Now I use them to catch problems before the patient even notices something’s off."AI Isn’t Coming-It’s Already in the Room
For years, many providers saw AI as a buzzword or a threat. Today, it’s a tool they can’t afford to ignore. Forrester’s 2025 report says AI is no longer optional-it’s part of the front line. That means algorithms helping triage patient messages, flagging potential sepsis from lab results hours before a human would, or suggesting treatment options based on a patient’s history and genetics. But adoption isn’t automatic. The biggest barrier isn’t cost or tech-it’s culture. Too many clinics still treat AI as something that replaces staff, not supports them. The real winners are the ones training their teams to use AI responsibly. That means teaching nurses how to spot biased algorithms, showing physicians how to audit AI recommendations, and rewarding staff who ask the right questions instead of punishing them for questioning the machine. IPG Health found that 52% of Americans now own a wearable device that tracks biometrics. Providers who ignore this data risk losing trust. Patients aren’t just coming in with data-they’re coming in with expectations. They want to know: "Did the AI look at my numbers? Did you check them?"
The Patient Is No Longer a Case-They’re a Partner
The old model of "doctor knows best" is fading fast. Today’s patients expect to co-design their care. They want options. They want transparency. They want to understand why a treatment was chosen over another. PwC calls this the "digital front door"-a seamless, 24/7 portal where patients can schedule visits, message providers, pay bills, and access their health records. But it’s more than tech. It’s a mindset shift. Providers who succeed are the ones who treat patients like collaborators. They ask, "What are your goals?" instead of "What’s wrong?" They use tools like virtual reality to help patients visualize how diabetes affects their kidneys, or how physical therapy can reduce knee pain. McKinsey’s 2025 Wellness Survey found that not all patients want to be deeply involved. Some are "wellness shirkers"-they just want the basics, and they’re price-sensitive. Others are "health enthusiasts" who track every step and meal. The best providers don’t treat everyone the same. They segment their approach. One patient gets a simple prescription. Another gets a personalized app with weekly check-ins and nutrition coaching.The Workforce Is Changing-And So Are the Rules
There’s a shortage of nurses, doctors, and technicians. But the real problem isn’t just fewer people-it’s fewer people who feel valued. Forrester reports that 53% of healthcare employers say retaining staff is their biggest challenge over the next five years. The solution? Certification matters more than ever. According to NHA’s 2025 Industry Outlook, 71% of employers have raised pay for staff who earn professional certifications. Medical assistants, phlebotomists, and pharmacy techs who get certified aren’t just more skilled-they’re more likely to stay. And that’s good for patients. When staff feel respected and invested in, care quality goes up. Clinics are also rethinking schedules. No longer do nurses have to be physically present for every virtual visit. Physicians are working from home or community centers. Teams are multidisciplinary: a nurse practitioner, a social worker, and a data analyst might all weigh in on a single patient’s care plan. This flexibility isn’t a perk-it’s a necessity to attract and keep talent.
It’s Not Just About Tech-It’s About Trust
Technology can do a lot. But it can’t replace human connection. IPG Health found that patients value authenticity over polished, AI-generated messages. A patient might not care if their appointment reminder came from a bot-but they’ll notice if the provider who answered their question sounded robotic or disengaged. The most successful providers are the ones blending tech with humanity. They use AI to handle routine tasks so they have more time to sit with patients. They use data to make better decisions but always follow up with a conversation: "What does this mean to you?" PwC’s research shows that providers building "health ecosystems" for patients with complex needs-like chronic illness, mental health struggles, or housing instability-are seeing better outcomes. These aren’t just clinics. They’re networks that connect patients with food programs, transportation help, and peer support-all coordinated by their care team.What This Means for Providers in 2025
If you’re a provider asking, "Do I need to change?"-the answer is yes. But you don’t need to become a tech expert overnight. Start small:- Ask patients if they use wearables or health apps-and what they’ve noticed.
- Learn how your clinic’s AI tools work. Don’t assume they’re flawless.
- Get certified if you haven’t. It’s not just for your resume-it’s for your team’s morale.
- Protect your time. Use tech to automate paperwork so you can focus on people.
- Listen more than you speak. Patients know more about their own bodies than ever before.
Are healthcare providers really using AI in daily practice yet?
Yes, and it’s growing fast. In 2025, over 60% of clinics in the U.S. and Australia use AI for tasks like triaging patient messages, flagging abnormal lab results, and predicting readmission risks. It’s not replacing doctors-it’s helping them work faster and catch issues earlier. The key is training staff to use it responsibly, not just relying on it blindly.
Do patients really care if their provider uses wearables or apps?
Absolutely. Nearly 70% of patients say they’re more likely to trust a provider who asks about their wearable data. It shows the provider is paying attention to details they care about. Patients aren’t just sharing data-they’re sharing their daily lives. Providers who ignore that miss a big part of the picture.
Why is certification becoming so important for healthcare staff?
Certification isn’t just about skills-it’s about retention. Employers are raising pay by 15-25% for certified staff because they see fewer errors, higher patient satisfaction, and lower turnover. In a field with 53% of employers struggling to keep staff, certification is one of the few proven ways to build loyalty and quality at the same time.
Can small clinics keep up with these changes?
Yes, but they need to be smart. You don’t need a $2 million tech system. Start with free or low-cost tools: use telehealth platforms that integrate with wearables, adopt open-source AI tools for appointment reminders, and partner with local community health groups. Focus on what matters most: building trust, reducing burnout, and listening to patients. Small clinics often do this better than big hospitals.
What’s the biggest mistake providers are making right now?
Trying to do everything at once. Many clinics rush into AI, digital portals, and new staffing models without fixing the basics: communication, team morale, and patient follow-up. The real win isn’t the shiny new tool-it’s making sure the person using it feels supported, and the patient feels heard.
14 Comments
Write a comment
More Articles
Anticholinergics and Urinary Retention: How Prostate Issues Make Medication Risks Worse
Anticholinergics for bladder issues can worsen urinary retention in men with prostate enlargement. Learn how these medications interact with BPH, the risks involved, and safer alternatives. Includes real-world data, expert advice, and management strategies.

Bipolar Disorder: Managing Mood Stabilizers and Antipsychotics Effectively
Effective management of bipolar disorder relies on mood stabilizers like lithium and antipsychotics such as quetiapine. Learn how these drugs work, their side effects, monitoring needs, and real-world trade-offs for long-term stability.
The Essential Guide to Salvia Divinorum: Everything You Need to Know About This Powerful Dietary Supplement
In my latest blog post, I delve into the fascinating world of Salvia Divinorum, a powerful dietary supplement that's been gaining popularity. I've compiled an essential guide, covering all the important aspects from its origin and benefits to side effects and safety measures. I've also touched on its legal status and how it can be used for various health-related purposes. This blog aims to provide a comprehensive understanding of Salvia Divinorum, making it easier for you to decide whether it's right for your dietary needs. Make sure to check it out if you're curious about this intriguing supplement!

Erin Nemo
November 30, 2025 AT 09:15My nurse practitioner asked me about my Apple Watch data last week and I actually felt seen for the first time. No more guessing games. She caught my resting heart rate spike before I even felt dizzy. Game changer.