When you pick up a generic pill at the pharmacy, you expect it to work just like the brand-name version. That’s not luck. It’s the result of one of the most tightly controlled processes in medicine. The U.S. Food and Drug Administration (FDA) doesn’t just approve generics because they’re cheaper. It approves them because they must meet the same exact standards for safety, quality, and strength as the original drug. There’s no room for guesswork.
What Makes a Generic Drug the Same?
The FDA doesn’t require generic manufacturers to repeat the expensive clinical trials that brand-name companies run. Instead, they use a shortcut called the Abbreviated New Drug Application (ANDA). But don’t let the word “abbreviated” fool you. This process is just as strict-it’s just smarter. The generic drug must contain the same active ingredient, in the same strength, same dosage form, and same route of administration as the brand-name drug. That’s the baseline.
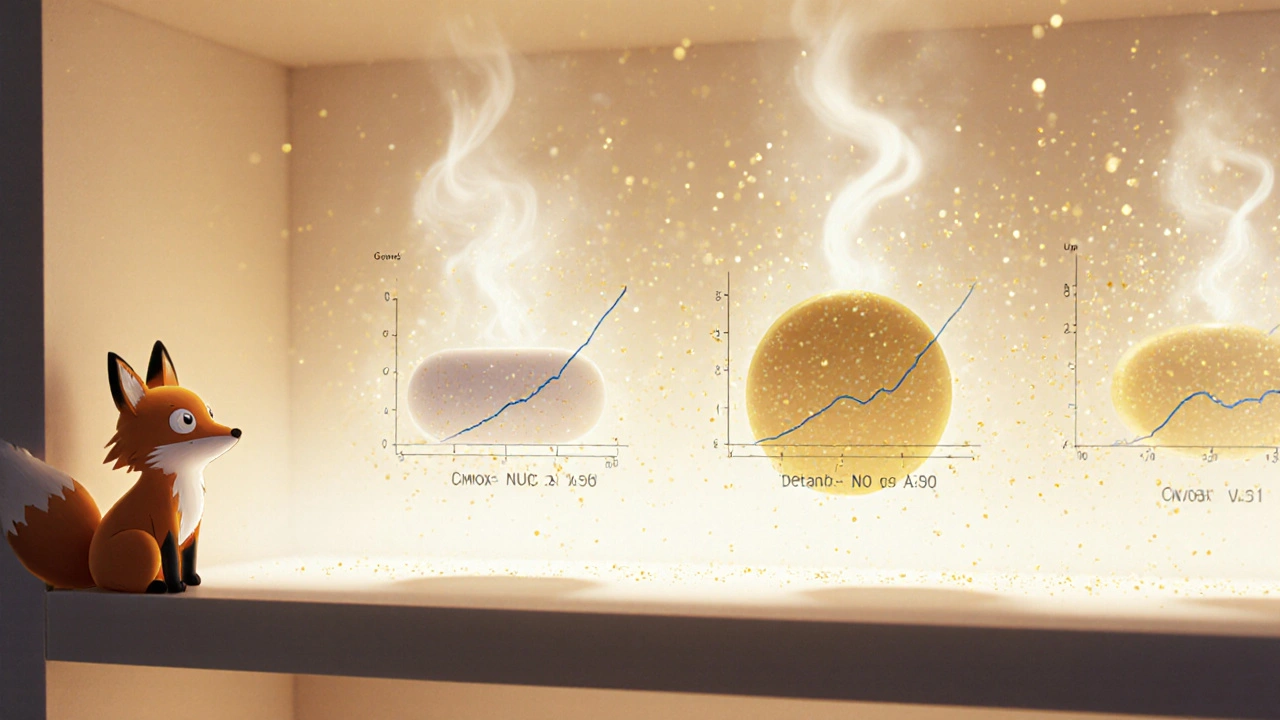
But here’s the catch: it’s not enough to have the same chemicals. The drug must behave the same way in your body. That’s where bioequivalence comes in. The FDA requires that the generic drug’s absorption rate falls within 80% to 125% of the brand-name drug’s. This range isn’t arbitrary. It’s based on decades of data showing that if a drug stays within this window, there’s no clinically meaningful difference in how it works. For most pills, this is tested in 24 to 36 healthy volunteers. Blood samples are taken over time to measure how much of the drug enters the bloodstream and how fast. The key numbers-Cmax and AUC-must match within those limits.
For complex drugs like extended-release tablets or inhalers, the rules get even tighter. Take Ritalin LA, for example. The FDA doesn’t just look at total absorption. It checks how the drug releases over time-first three hours, then three to seven, then seven to twelve. If the generic releases too fast or too slow, it won’t work the same. That’s why only 58% of complex generic applications get approved within three tries, compared to 76% for simple pills.
Quality Isn’t Optional-It’s Built In
Generic drugs aren’t made in backrooms. They’re made in factories inspected by the FDA. Every facility must follow Current Good Manufacturing Practices (cGMP), which are federal rules written in 21 CFR Parts 210 and 211. These rules cover everything: how ingredients are stored, how machines are cleaned, how batches are tested. The FDA does about 1,200 pre-approval inspections every year. If a factory has inconsistent tablet hardness, like Hetero Labs did with its generic Jardiance in 2021, the application gets rejected. No second chances.
Manufacturers have to prove consistency across at least three full-scale production batches. It’s not enough to make one perfect batch in the lab. The process must work every single time, at volume. That’s why many companies hire teams with five or more years of ANDA experience. A typical application runs 5,000 to 10,000 pages long-chemistry data, manufacturing details, stability tests, labeling. Every page matters.
Even the inactive ingredients-fillers, dyes, coatings-must be safe and consistent. The FDA tracks these too. If a generic uses a different coating that changes how fast the pill dissolves, it fails. It’s not about cost. It’s about control.
Strength Isn’t Just a Number
When a pill says “10 mg,” it doesn’t mean “about 10 mg.” It means exactly 10 mg, plus or minus a tiny, scientifically defined margin. The FDA requires manufacturers to prove the strength of each batch within strict limits. For most drugs, that’s ±5%. For drugs with a narrow therapeutic index-like warfarin, lithium, or levothyroxine-the margin is even tighter.
Levothyroxine, used for thyroid conditions, is a perfect example. Even small changes in dosage can cause serious side effects. So in 2020, the FDA updated its guidance to require a 95% to 105% bioequivalence range for generic levothyroxine. That’s tighter than the standard 80%-125%. And it’s not just a suggestion. Manufacturers had to retest every batch. Some were pulled from the market until they met the new standard.
This isn’t about being overly cautious. It’s about protecting patients who rely on these drugs every day. A 10% variation in warfarin might mean the difference between a clot and a bleed. The FDA doesn’t take that risk lightly.

Why Do So Many Generics Get Rejected?
You’d think with a shorter path, approvals would be faster. But that’s not the case. Less than 10% of generic applications get approved on the first try. Why? Because the bar is set high, and many applicants underestimate how detailed the FDA expects them to be.
Common reasons for rejection:
- Missing or incomplete bioequivalence data
- Inconsistent manufacturing processes
- Insufficient stability testing
- Improper labeling or packaging
- Failure to address FDA’s Question-Based Review (QbR) requirements
The QbR system, introduced in 2005 and updated in 2018, forces manufacturers to think like regulators. Instead of just submitting data, they have to explain why each step matters. What’s the critical quality attribute? How do you know it’s controlled? What happens if the temperature changes during storage? If the answer isn’t clear, the application gets a Complete Response Letter-and the clock resets.
Companies that succeed early use the FDA’s Pre-ANDA program. About 78% of approved applicants meet with FDA staff before submitting. These meetings aren’t optional-they’re strategic. They help avoid costly mistakes.
How Long Does It Take? How Much Does It Cost?
Bringing a simple generic to market takes about 32.7 months on average. For complex drugs like inhalers or injectables, it can stretch to 47 months. The cost? Around $1.3 million for a standard pill. For a complex product like an epinephrine auto-injector, it can hit $25 million. Compare that to the $2.6 billion it takes to develop a new brand-name drug, and you see why generics are so important.
The FDA aims to review standard applications within 10 months. Priority reviews are done in 8. And they’re hitting those targets-95% of reviews are completed on time. But the real win isn’t speed. It’s savings. In 2022, generics saved the U.S. healthcare system $373 billion. That’s $1.7 trillion over the next decade, according to the Congressional Budget Office.

What About Complex Drugs?
Not all generics are created equal. Simple tablets? Easy. Inhalers? Hard. Topical creams? Even harder. Why? Because with these drugs, the delivery system is part of the medicine. The device matters as much as the chemical.
The EpiPen is a classic example. Between 2015 and 2020, the FDA approved only 3 out of 27 generic applications. Why? Because the auto-injector’s spring mechanism, needle length, and pressure had to match the original exactly. A tiny difference could mean the drug doesn’t reach the muscle. The FDA had to create new testing standards just for these devices.
Now, the agency is targeting 127 complex products with no generics yet-worth $52 billion in annual sales. These include long-acting injectables, nasal sprays, and specialized creams. The FDA’s 2023 draft guidance on complex generics shows they’re serious about closing this gap. By 2027, they want half of these complex applications approved within two review cycles.
Are Generics Really Safe?
Yes. And the data proves it. A 2021 report from the American Medical Association reviewed 15 years of real-world use and found that 98.7% of generic drugs performed identically to brand-name drugs in clinical outcomes. Post-market surveillance shows no spike in side effects or treatment failures.
Dr. Janet Woodcock, former head of the FDA’s drug center, put it simply: “Every approved generic meets the same rigorous standards as the brand-name drug.”
Some critics point to the 80%-125% bioequivalence range as too wide. But the FDA already tightens it for high-risk drugs. For levothyroxine, it’s 95%-105%. For some antiepileptics and blood thinners, it’s 90%-111%. The system adapts to the risk.
The real issue isn’t safety-it’s access. Patent tricks and legal delays often block generics from reaching the market for years after approval. The FTC found that, on average, generics wait 2.4 years after FDA approval before they can actually be sold. That’s not a science problem. That’s a legal one.
But when generics do get through, they work. And they save lives. Every day, 90% of prescriptions filled in the U.S. are generics. And they’re not second-rate. They’re science-backed, rigorously tested, and just as effective.
Are generic drugs as safe as brand-name drugs?
Yes. The FDA requires generic drugs to meet the same strict standards for safety, strength, quality, and purity as brand-name drugs. They must contain the same active ingredient and prove they work the same way in the body through bioequivalence testing. Over 98% of generic drugs show no clinically meaningful difference in outcomes compared to their brand-name counterparts, according to long-term post-market data.
Why do some generic drugs get rejected by the FDA?
Most rejections happen because the manufacturer didn’t meet the FDA’s exacting standards for bioequivalence, manufacturing consistency, or documentation. Common issues include inconsistent tablet hardness, incomplete stability data, or failure to address the FDA’s Question-Based Review (QbR) requirements. Even small deviations in how a drug releases or is packaged can lead to a Complete Response Letter.
How does the FDA test if a generic drug works the same as the brand-name version?
The FDA uses bioequivalence studies, where healthy volunteers take both the generic and brand-name drug. Blood samples are taken over time to measure how much of the drug enters the bloodstream and how fast. Key measurements-Cmax and AUC-must fall within 80%-125% of the brand-name drug’s values. For complex drugs like extended-release tablets or inhalers, additional tests track how the drug releases over time.
Are all generic drugs made in the U.S.?
No. Most generic drugs are manufactured overseas, primarily in India and China. But every facility-whether in the U.S., India, or elsewhere-must pass the same FDA inspections. The FDA conducts over 1,200 pre-approval inspections annually, and half of those are overseas. If a factory fails an inspection, the application is delayed until the issues are fixed.
Can a generic drug have different side effects than the brand-name version?
The active ingredient is identical, so the side effects should be the same. However, differences in inactive ingredients-like dyes or fillers-can rarely cause allergic reactions in sensitive individuals. These are listed on the label. If you notice a new reaction after switching to a generic, talk to your doctor. But the core drug’s effects, both therapeutic and adverse, are the same.
How long does it take for a generic drug to be approved?
For a standard oral tablet, the FDA aims to complete its review within 10 months of submission. But the whole process-from developing the drug to submitting the application-usually takes 32.7 months on average. Complex drugs like inhalers or injectables can take over 47 months. Many applications are rejected on the first try, which adds time.
Why are generic drugs so much cheaper?
Generic manufacturers don’t have to repeat expensive clinical trials. They rely on the brand-name drug’s safety and efficacy data. Their main costs are in proving bioequivalence and meeting manufacturing standards. The average cost to develop a generic is $1.3 million, compared to $2.6 billion for a new brand-name drug. This allows generics to be sold at a fraction of the price-saving patients and the healthcare system hundreds of billions each year.
What’s Next for Generic Drugs?
The FDA is pushing harder than ever to bring more complex generics to market. The 2023 GDUFA III plan sets a goal: approve half of complex generic applications within two review cycles by 2027. That’s up from just 28% today. New approvals like the first generic of Humira in late 2023 show progress is possible-even for the toughest drugs.
But the real challenge isn’t science. It’s access. Patent extensions, legal battles, and pay-for-delay deals still block generics from reaching patients for years after approval. The FDA can’t fix that. But it can make sure that when a generic does get through, it’s just as safe, strong, and reliable as the brand.
And that’s the point. You don’t have to choose between cost and quality. With generics, you get both.
10 Comments
Write a comment
More Articles

Constipation from Medications: How to Manage It Without Stopping Your Prescriptions
Constipation from medications is common but often ignored. Learn how to manage it safely without stopping your prescriptions, using proven laxatives, avoiding harmful fixes, and knowing when to ask for stronger help.

Julie Pulvino
November 23, 2025 AT 11:05Just got my generic levothyroxine refill and honestly? Zero difference. I’ve been on it for 8 years. My TSH is rock steady. The FDA knows what they’re doing. No need to overpay for the brand.