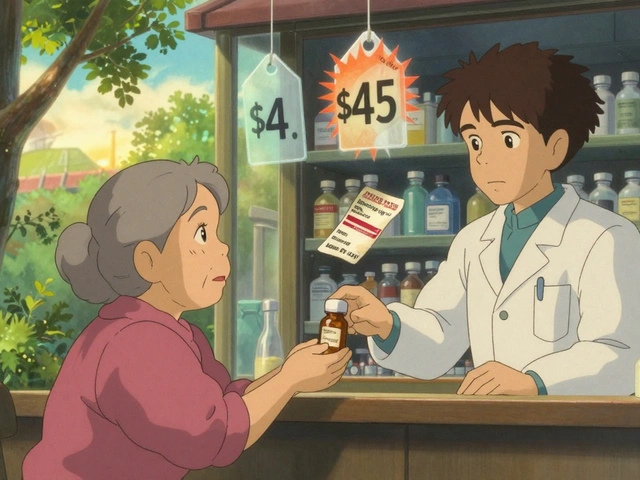
For someone who’s had a kidney, liver, or heart transplant, staying alive means taking medication every single day-forever. And those meds? They’re expensive. Brand-name drugs like Prograf or CellCept can cost over $2,000 a month. That’s not just a burden-it’s a barrier. But there’s a proven, affordable alternative: generic immunosuppressive combinations. These aren’t second-rate options. They’re the same active ingredients, rigorously tested, and now used by the majority of new transplant patients in the U.S.
What Are Generic Immunosuppressive Combinations?
After a transplant, your body tries to reject the new organ. Immunosuppressants stop that. The standard approach is a triple combo: a calcineurin inhibitor (like tacrolimus or cyclosporine), an antimetabolite (like mycophenolate), and sometimes corticosteroids. For years, only brand-name versions were available. Now, nearly all of them have generic equivalents.
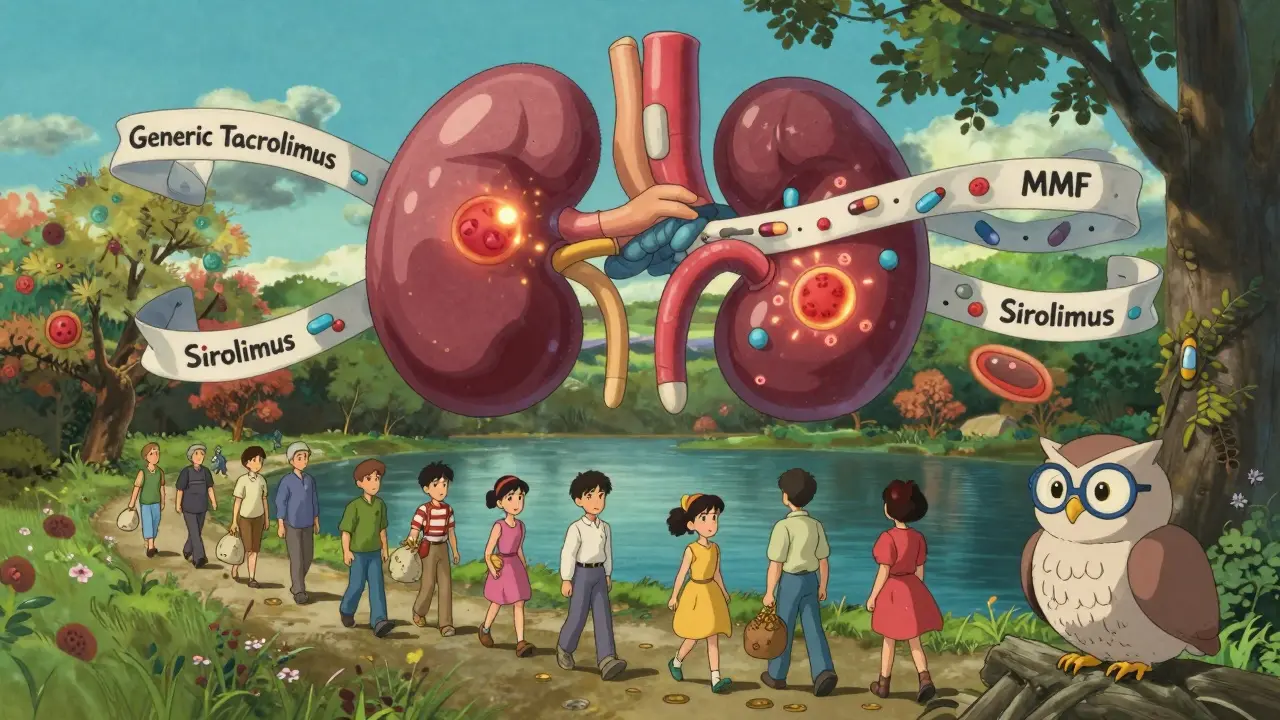
Generic tacrolimus hit the market in 2015 after Prograf’s patent expired. Generic mycophenolate mofetil (MMF) followed in 2019. By 2020, sirolimus and mycophenolic acid (MPA) were also available as generics. Today, over 78% of new kidney transplant prescriptions are for these generic versions, according to IQVIA data from 2023.
These aren’t just cheaper copies. They’re required by the FDA to match the brand-name drug’s performance within strict bioequivalence limits-80% to 125% of the original’s absorption. For most drugs, that’s fine. But immunosuppressants are different. They work in a razor-thin zone. Too little, and your body rejects the organ. Too much, and you risk kidney damage, infection, or even cancer.
Cost Savings Are Real-But Not Automatic
The math is simple. Brand-name tacrolimus costs $1,800 to $2,200 a month. Generic? $300 to $400. That’s an 80% drop. For MMF, the savings are even steeper: $1,500 down to $200. Over a year, that’s $18,000 to $20,000 saved per person. Multiply that by 40,000 transplants a year in the U.S., and you’re looking at nearly $1 billion in annual savings for the healthcare system.
But savings don’t happen just by switching pills. A 2022 study in the American Journal of Transplantation found that while graft survival rates were nearly identical between brand and generic tacrolimus (95.1% vs. 94.7%), 12% of patients needed dose adjustments in the first three months. Why? Because even small differences in how the body absorbs the drug can throw blood levels out of range.
One patient on Reddit, who went by ‘TransplantSurvivor89,’ switched to generic tacrolimus in 2022 and saved $1,500 a month-but had three rejection episodes in the first year. He ended up going back to the brand. Another, ‘KidneyWarrior2020,’ used generic MMF for three years with zero issues and saved over $18,000. The difference? Monitoring.
Monitoring Is Non-Negotiable
There’s no such thing as a set-and-forget generic immunosuppressant. You need regular blood tests. For tacrolimus, the target range is 5-10 ng/mL. For sirolimus, it’s 100-150 ng/mL. For MMF, it’s 1.0-1.5 mg/L. If your level drops below that, rejection risk spikes. If it goes above, toxicity kicks in.
Transplant centers now require biweekly blood draws for the first month after switching to a generic, then monthly for at least six months. Some pharmacists report a 30% increase in clinic visits during the first six months after conversion. That’s not a failure-it’s part of the process.
And it’s not just about the drug itself. Interactions matter. A 2023 study in the Journal of Antimicrobial Chemotherapy found that 67% of transplant patients on multiple immunosuppressants had at least one dangerous drug interaction-often with antibiotics, antifungals, or even grapefruit juice. Generic versions don’t change that. They just make it easier to overlook because they’re cheaper and more common.
Which Combinations Work Best?
Not all combos are created equal. The most common is tacrolimus + MMF. It’s used in 64% of kidney transplants. But other combinations have their place.
Sirolimus + tacrolimus is underused. A 2019 analysis from the University of Maryland, based on UNOS data, showed lung transplant patients on this combo lived a median of 8.9 years-compared to 7.1 years on tacrolimus + MMF. The catch? Sirolimus doesn’t work well if you’ve had recent surgery or have poor wound healing. It also raises cholesterol and can cause mouth sores.
Then there’s the steroid-sparing approach. Corticosteroids like prednisone cause weight gain, diabetes, and bone loss. A 2024 review in Transplantation Reviews found that using generic tacrolimus with sirolimus instead of steroids cut the risk of post-transplant diabetes by 31%. For patients already at risk for diabetes, this combo isn’t just cheaper-it’s healthier.
But here’s the kicker: switching to a new combo isn’t something you do on your own. It requires a transplant team that knows the nuances. One pharmacist in a 2022 Journal of Pharmacy Practice article said, “We see 30% more clinic visits in the first 6 months after generic conversion due to level fluctuations.” That’s not a flaw in the drugs-it’s a flaw in how some centers handle the transition.
Manufacturing Quality and Consistency
Not all generics are made the same. The FDA allows a 80-125% bioequivalence range. That’s a 45% window. For a drug like tacrolimus, where 1 ng/mL can mean the difference between safety and rejection, that’s a problem. In 2022, the FDA’s own inspections found 12% of generic tacrolimus batches failed USP dissolution testing-meaning they didn’t release the drug properly in the gut.
That’s why 85% of transplant centers now require all patients to stay on the same generic manufacturer. If you start on Teva’s tacrolimus, you stay on Teva’s. Switching between manufacturers-even if both are “generic”-can cause blood levels to swing wildly. One patient might be stable on Mylan’s version, then crash after switching to Sandoz’s. It’s not the drug. It’s the formulation.
Transplant centers have learned to lock in one supplier. Patients get their prescriptions filled at the same pharmacy, every time. No substitutions. No surprises.
What Experts Say
Dr. Lloyd Ratner from Columbia University put it plainly in a 2022 editorial: “Generic immunosuppressants, when used with appropriate therapeutic drug monitoring, provide equivalent outcomes at a fraction of the cost.”
But not everyone agrees. Dr. Jean Emond from NewYork-Presbyterian warned in a 2023 Medscape interview that the FDA’s 80-125% range is “too broad for narrow therapeutic index drugs.” She’s not wrong. The FDA itself acknowledged this in 2022 and started pushing for tighter standards-90-111%-for immunosuppressants.
Meanwhile, the American Society of Transplantation updated its guidelines in 2021 to say: “Generic substitution is acceptable, but only with close monitoring and patient education.” Translation? It’s safe-if you do it right.
Who Should Avoid Generics?
Most patients can switch safely. But some shouldn’t. If you’ve had a recent rejection episode, or if your blood levels have been unstable in the past, switching to a generic might be risky. Same if you’re on multiple medications that interact with immunosuppressants-like certain antifungals or HIV drugs.
Patients with kidney or liver problems also need extra caution. These organs help break down the drugs. If they’re not working well, even small changes in absorption can be dangerous.
And if you’ve been on the same brand-name drug for 10 years with perfect stability? Sometimes, the best move is to stay put. If it ain’t broke, don’t fix it-especially if you’re not facing financial hardship.
The Future: Better, Cheaper, Smarter
The trend is clear. In 2016, only 15% of new kidney transplants used generic tacrolimus. By 2023, it was 82%. The market is growing at nearly 10% a year. The FDA’s 2023 approval of the first interchangeable biosimilar for belatacept (Nulojix) is a sign of things to come. Biosimilars are even more precise than generics-they’re almost identical to the original biologic.
And new guidelines from KDIGO in 2024 now recommend generic sirolimus as a first-line option for high-risk kidney transplant patients. That’s huge. It means experts are moving beyond just cost and into real clinical strategy.
Long-term, the goal isn’t just to cut costs. It’s to use these cheaper drugs to enable new treatments-like protocols that might one day let patients stop immunosuppressants entirely. A clinical trial (NCT00078559) is already testing whether a strong initial treatment with alemtuzumab, followed by generic tacrolimus and sirolimus, can train the immune system to accept the transplant without lifelong drugs.
That’s the future. But for now, the present is simple: generic immunosuppressants work. They’re safe. They’re effective. And they’re saving lives-by making survival affordable.
What You Need to Do If You’re Switching
- Don’t switch on your own. Talk to your transplant team. This isn’t a pharmacy decision-it’s a medical one.
- Ask for consistency. Make sure you get the same generic brand every time. No switching between manufacturers.
- Expect more blood tests. Biweekly for the first month, then monthly for six months. This isn’t extra-it’s essential.
- Track your symptoms. Fever, fatigue, swelling, or unusual bruising? Call your team immediately. Don’t wait.
- Know your drug interactions. Tell every doctor, pharmacist, and even your dentist you’re on immunosuppressants. Even OTC meds can interfere.
- Use patient support programs. Sixty-five percent of generic manufacturers now offer copay assistance. Don’t assume you’re on your own.
Are generic immunosuppressants as effective as brand-name drugs?
Yes, when used correctly. Multiple studies, including a 2022 analysis in the American Journal of Transplantation, show that one-year graft survival rates with generic tacrolimus are nearly identical to brand-name-94.7% versus 95.1%. The key is consistent dosing and regular blood monitoring. Without those, effectiveness drops.
Can I switch from brand to generic on my own?
No. Switching immunosuppressants without medical supervision is dangerous. Even small changes in absorption can trigger rejection or toxicity. Always work with your transplant team. They’ll adjust your dose and schedule blood tests to ensure your levels stay in the safe range.
Why do some patients have rejection episodes after switching to generics?
It’s usually due to inconsistent blood levels. Generic drugs must meet FDA bioequivalence standards (80-125%), but that’s a wide range. If your body absorbs the generic version differently than the brand, your drug levels can drop too low. This is why frequent blood tests are required after switching. Most rejection episodes happen in the first three months when monitoring isn’t tight enough.
Which generic immunosuppressants are available today?
Generic versions are now available for tacrolimus, cyclosporine, mycophenolate mofetil (MMF), mycophenolic acid (MPA), and sirolimus. These cover the core drugs used in most transplant regimens. Sirolimus and MPA generics became widely available in 2020. Newer biosimilars, like the one approved for belatacept in 2023, are starting to appear and may offer even better consistency.
Is it safe to switch between different generic brands?
No. Even though two drugs are both labeled “generic tacrolimus,” different manufacturers use different fillers and manufacturing processes. These can affect how the drug is absorbed. Most transplant centers require patients to stay on the same generic brand for life to avoid dangerous fluctuations in blood levels.
How do I know if my generic immunosuppressant is working?
You won’t feel it. That’s the problem. The only way to know is through regular blood tests that measure drug levels (trough levels). For tacrolimus, your level should stay between 5-10 ng/mL. For sirolimus, it’s 100-150 ng/mL. If your levels are outside that range, your transplant team will adjust your dose. Never rely on how you feel.
Are there any long-term risks with using generic immunosuppressants?
The long-term risks are the same as brand-name drugs: higher chance of infection, kidney damage, or cancer. The drugs themselves don’t change. The risk comes from inconsistent dosing. If your blood levels fluctuate because you switched manufacturers or missed monitoring, your risk goes up. Sticking to one brand and following your monitoring schedule reduces this risk significantly.
Can I save money with generics even if I have insurance?
Absolutely. Even with insurance, copays for brand-name immunosuppressants can be $500-$1,000 a month. Generic versions often cost under $50 with insurance, and sometimes $0 with manufacturer assistance programs. CMS requires Medicare Part D to cover all transplant immunosuppressants, so most patients have access. The real savings come from avoiding hospitalizations due to rejection or toxicity-something generics help prevent when used properly.
15 Comments
Write a comment
More Articles

Improve Your Health and Vitality with Phleum Pratense Dietary Supplements
In my latest blog post, I delve into the health benefits of Phleum Pratense dietary supplements. Also known as Timothy Grass, this supplement has been linked to improved overall vitality and health. It's rich in antioxidants and can help boost immunity and soothe respiratory issues. I've also explored the potential for this supplement to aid in digestion and manage allergies. I strongly recommend giving it a try if you're looking to enhance your health naturally.

clarissa sulio
February 2, 2026 AT 08:01Generics are the only way forward in this country. We pay too much for everything already. If the FDA says they’re equivalent, trust the science. No one needs to be paying $2k a month for pills that do the same thing.