
Why Your Itchy Skin After an Opioid Might Not Be an Allergy
It’s common to get itchy after taking morphine or codeine. Many people assume this means they’re allergic. But here’s the truth: itching from opioids is rarely a true allergy. In fact, up to 80% of people who say they’re allergic to opioids are actually having a pseudoallergic reaction - a side effect, not an immune response. This misunderstanding leads to unnecessary avoidance of powerful painkillers, worse pain control, and higher medical costs. You might be labeled "allergic" just because you scratched your arm after a hospital dose - but that doesn’t mean you can’t safely use other opioids.
The Difference Between True Allergy and Pseudoallergy
A true opioid allergy involves your immune system. It’s rare - affecting only about 0.1% to 0.3% of people who take opioids. Signs include hives, swelling of the lips or tongue, trouble breathing, a drop in blood pressure, or a widespread rash. These reactions usually happen fast - within minutes - and can be life-threatening. If you’ve ever passed out or needed epinephrine after an opioid, that’s a true allergy.
Most opioid reactions are pseudoallergies. These aren’t immune-driven. Instead, the opioid directly triggers mast cells in your skin to dump histamine. Think of it like poking a hornet’s nest - the hornets (histamine) fly out, but no one actually attacked them. The result? Itching, flushing, sweating, mild dizziness, or sneezing. These symptoms are uncomfortable, but not dangerous. They often get worse with higher doses or faster IV pushes. Morphine is the worst offender - it releases 3 to 4 times more histamine than hydromorphone or fentanyl per milligram.
Why Morphine Makes You Itch - And Why Fentanyl Doesn’t
Not all opioids are created equal when it comes to itching. Morphine and codeine, both natural opioids, have a chemical structure that easily triggers histamine release. That’s why up to 40% of people on morphine report itching. Synthetic opioids like fentanyl, methadone, and oxycodone are much less likely to cause it. Fentanyl, for example, needs 10 times more concentration than morphine to trigger the same reaction. That’s why many patients who can’t tolerate morphine do fine on a fentanyl patch.
Even more interesting: itching from opioids isn’t always about histamine. A 2007 study from Washington University found that opioids activate a specific receptor in the spinal cord called GRPR. This pathway causes itching independently of histamine. That’s why antihistamines like Benadryl sometimes don’t fully help - they’re treating the wrong part of the problem.
What to Do If You Get Itchy on an Opioid
If you start itching after an opioid, don’t panic. Don’t assume you’re allergic. Here’s what actually works:
- Lower the dose. Reduce your opioid by 25-50%. Many people find itching disappears at lower doses.
- Try an antihistamine. Take diphenhydramine (Benadryl) 25-50 mg orally or IV 30 minutes before your next dose. It helps in 80-90% of cases.
- Switch opioids. If itching continues, move to a low-histamine opioid. Fentanyl patches or methadone are top choices. Fentanyl causes itching in only 10-15% of users. Methadone? Even lower.
- Don’t stop opioids entirely. Unless you have swelling, breathing issues, or low blood pressure, there’s no need to avoid all opioids. You’re not allergic - you just need a different one.
Many cancer patients and chronic pain sufferers have been told they’re "allergic to all opioids" because they got itchy on morphine. But studies show that over 75% of these patients can safely use fentanyl or methadone with antihistamine support. One Harvard study found 78% of cancer patients with "opioid allergy" labels tolerated alternative opioids after proper management.
When You Actually Have a Real Allergy
True opioid allergies are rare, but they’re serious. If you’ve ever had:
- Sudden swelling of the face, throat, or tongue
- Wheezing or trouble breathing
- Passing out or a sudden drop in blood pressure
- A widespread, blistering rash
- then you need to avoid that opioid and any closely related ones. Morphine, oxycodone, and hydrocodone are all phenanthrene opioids and can cross-react. But fentanyl, methadone, and tramadol are structurally different and rarely cause cross-reactions. If you’ve had a true allergic reaction, your doctor may recommend a skin test or a supervised challenge with a different opioid to confirm.

Why This Matters - And How It’s Changing
Mislabeling opioid allergies is a huge problem. In the U.S., about 10-15% of people on opioids say they’re allergic. That’s 20-30 million people annually. But studies show 90% of those labels are wrong. This leads to:
- Use of less effective, more expensive painkillers
- Increased risk of opioid misuse due to inadequate pain control
- $1,200 more in medication costs per patient
- Over $30 billion extra spent nationwide each year
Hospitals are starting to fix this. Epic’s electronic health records now flag "itching" separately from "allergy." Clinics are using tools like the Opioid Allergy Assessment Tool, which correctly identifies pseudoallergies in 92% of cases. The American Academy of Allergy, Asthma & Immunology now recommends against routine skin testing unless anaphylaxis occurred. Instead, they suggest a trial with a different opioid under observation.
New Treatments on the Horizon
Science is catching up. In 2023, a new drug called nalfurafine - approved in Japan since 2009 - showed 70% reduction in opioid-induced itching in U.S. trials without reducing pain relief. It works by targeting the spinal GRPR pathway, not histamine. The FDA is reviewing it for approval.
Researchers are also looking at genetic markers. Some people have variations in the HTR7 gene that make them more likely to release histamine when taking opioids. In the future, a simple blood test might tell you if you’re at high risk for itching - and which opioid to avoid.
Two new opioid candidates, CR845 and NOP receptor agonists, are in late-stage trials. They’re designed to relieve pain without triggering itching at all. Early results show an 80% drop in pruritus.
What Patients Should Know
If you’ve been told you’re allergic to opioids because you got itchy:
- Don’t accept that label without questions.
- Write down exactly what happened: Was it just itching? Did you swell? Could you breathe?
- Ask your doctor: "Could this be a side effect, not an allergy?"
- Ask if you can try fentanyl or methadone with Benadryl first.
- Don’t self-treat with OTC antihistamines long-term - talk to a provider.
And if you’ve had a real allergic reaction - swelling, breathing trouble - make sure your medical records reflect that clearly. Wear a medical alert bracelet if needed. But for the vast majority of people: itching doesn’t mean you’re allergic. It just means you need a different approach.
Is itching from opioids a sign of a true allergy?
No, itching alone is rarely a true allergy. It’s usually a pseudoallergic reaction caused by histamine release from mast cells, not an immune response. True allergies involve swelling, trouble breathing, low blood pressure, or hives. If you only get itchy, you’re likely not allergic - you just need a different opioid or an antihistamine.
Which opioids cause the most itching?
Morphine and codeine cause the most itching because they strongly trigger histamine release. Up to 40% of people on morphine report itching. Fentanyl, methadone, and oxycodone cause significantly less - only 10-15% of users. Hydromorphone is also a good alternative with low histamine-releasing potential.
Can I still take opioids if I get itchy?
Yes. Most people who get itchy on one opioid can tolerate another. Switching to fentanyl, methadone, or hydromorphone often solves the problem. Adding an antihistamine like diphenhydramine before dosing helps in 80-90% of cases. Avoiding all opioids because of itching can lead to worse pain and higher risks of misuse.
Should I get tested for an opioid allergy?
Only if you had a severe reaction like anaphylaxis (swelling, breathing trouble, passing out). Skin tests for opioids are unreliable and often give false positives. Most experts recommend a supervised trial with a different opioid instead of testing. The American Pain Society advises against routine skin testing.
What’s the safest opioid if I’m sensitive to itching?
Fentanyl and methadone are the safest choices for people prone to itching. Fentanyl has very low histamine-releasing activity and is often used in patches for chronic pain. Methadone rarely causes itching and is effective for long-term pain. Both require careful dosing - fentanyl is very potent, and methadone has a long half-life - so they should be started under medical supervision.
Can I take Benadryl with opioids to stop itching?
Yes, diphenhydramine (Benadryl) is commonly used to prevent or reduce opioid-induced itching. Take 25-50 mg 30 minutes before your opioid dose. It works best for histamine-related itching but may not help if the itching comes from spinal GRPR activation. It’s safe for short-term use, but avoid long-term daily use due to drowsiness and other side effects.
9 Comments
Write a comment
More Articles

Living with Dyskinesia: Real‑World Impact on Daily Life
A personal look at how dyskinesia affects daily routines, work, and relationships, plus practical tips, treatment options, and future developments for those living with Parkinson's movement disorders.
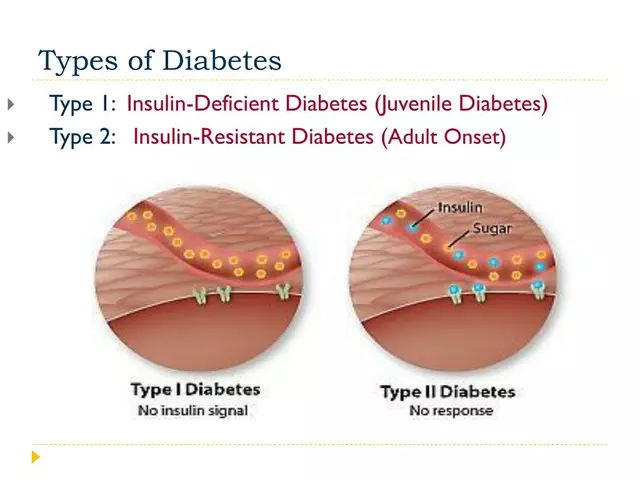
How Saxagliptin Affects Insulin Resistance in Type 2 Diabetes
As a blogger focused on health and wellness, I recently came across some interesting research on how Saxagliptin affects insulin resistance in Type 2 Diabetes. From what I've gathered, Saxagliptin is a medication that helps to control blood sugar levels by increasing the release of insulin and reducing the amount of glucose produced by the liver. This ultimately results in better management of Type 2 Diabetes and improved overall health. I was impressed to learn that this medication can not only help those struggling with insulin resistance but also reduce the risk of long-term complications associated with diabetes. I'm eager to continue following this topic and sharing more insights with my readers.

Revitalize Your Health with the Magic of European Mistletoe – Nature's Best-Kept Secret
In my latest blog, I delve into the sheer magic of European Mistletoe, nature's best-kept secret for revitalizing health. I was amazed to uncover a host of benefits from this humble plant, including boosting immune function and aiding in cancer treatment. I've also found out that it's been used for centuries in Europe for various medicinal purposes. It's incredible how this underestimated plant can be a game-changer for our well-being. So, join me as I explore and share the powerful benefits of the European Mistletoe for your health.

Shawn Daughhetee
November 23, 2025 AT 21:15I got itchy after morphine once and thought I was gonna die. Turned out I just needed Benadryl and switched to fentanyl. No more itching, no more drama. Why do people make this so complicated?