
When your bones start to weaken without you noticing, it’s not just about getting older-it’s a real medical issue. Osteoporosis isn’t a normal part of aging. It’s a disease where your body loses bone faster than it can rebuild it, leaving bones thin, brittle, and dangerously prone to breaking from minor falls-or even from sneezing. This isn’t rare. In the U.S. alone, about 10 million people have osteoporosis, and another 44 million are on the brink with low bone density, called osteopenia. For women over 50, the risk is especially high. After menopause, estrogen drops, and that’s when bone loss can accelerate sharply. But men aren’t immune. One in four men over 50 will break a bone due to osteoporosis. The real danger? These fractures often happen in the hip, spine, or wrist, and they can change your life forever.
What Happens Inside Your Bones?
Your bones aren’t static. They’re alive, constantly being broken down and rebuilt. Special cells called osteoclasts chew away old bone, while osteoblasts lay down new bone. In healthy adults, these two processes balance out. But with osteoporosis, the balance tips. Osteoclasts get too active, and osteoblasts can’t keep up. Over time, your bone’s internal structure becomes porous, like a sponge with holes. This isn’t just about density-it’s about architecture. The trabecular network inside your bones-the spongy part that absorbs shock-starts to thin and disconnect. That’s why a fall from standing height can lead to a broken hip. A simple cough can collapse a vertebra. And once you’ve had one fracture, your risk of another skyrockets.
Why Bisphosphonates Became the Go-To Treatment
For decades, doctors had few tools to stop bone loss. Then came bisphosphonates. These drugs don’t build bone-they stop it from being destroyed. First developed in the 1980s, they’ve since become the most prescribed osteoporosis medication in the world. The reason? They work. And they’re affordable. Bisphosphonates bind to bone surfaces and target osteoclasts. Once inside, they disrupt the cells’ energy production, essentially putting them to sleep or killing them off. Fewer osteoclasts mean less bone breakdown. The result? Bone density improves by 5% to 10% over three years, and fracture risk drops dramatically.
Alendronate (Fosamax), for example, cuts vertebral fractures by 48% and hip fractures by 51% over three years, according to the landmark Fracture Intervention Trial. Zoledronic acid (Reclast), given as a yearly IV infusion, works just as well and avoids stomach issues. These aren’t just numbers-they’re real outcomes. People who take bisphosphonates are far less likely to end up in a hospital after a fall, or need surgery for a broken spine.
How They’re Taken-and Why It Matters
Not all bisphosphonates are the same. There are two main types: oral and intravenous. Oral versions like alendronate, risedronate, and ibandronate are taken once a week or once a month. But they’re fussy. You have to take them first thing in the morning, with a full glass of plain water. No coffee, no juice, no food. Then you have to stay upright for at least 30 minutes-no lying down, no slouching. Why? Because if the pill sits in your esophagus, it can cause serious irritation, even ulcers. Many patients stop taking them because of this. Studies show only about 50% to 70% stick with oral bisphosphonates after a year.
That’s where the IV option comes in. Zoledronic acid is given once a year in a doctor’s office. No fasting. No waiting upright. Just a 15-minute infusion. For people who can’t tolerate the pills, or who forget to take them, this is a game-changer. It’s also more effective at raising bone density in some cases. But it’s not without risks-some people get flu-like symptoms for a day or two after the infusion.

The Hidden Risks and Long-Term Concerns
Nothing in medicine is perfect. Bisphosphonates are powerful, but they come with rare, serious side effects. One is atypical femoral fractures-unusual breaks in the thigh bone that happen without trauma. These are extremely rare: about 3 to 5 cases per 10,000 patient-years. Another is osteonecrosis of the jaw, where bone tissue in the mouth dies. That happens in roughly 1 in 10,000 patients. Both are more likely in people who’ve been on bisphosphonates for more than five years, or those with dental problems or cancer.
That’s why guidelines now recommend a “drug holiday.” After three to five years of treatment, especially if your fracture risk has gone down and your bone density has stabilized, your doctor might suggest stopping the medication for a while. Your bones retain some of the drug’s effects even after you stop. During the break, you’ll still get regular bone density scans. If your risk rises again, you can restart. This approach balances long-term protection with minimizing rare side effects.
How Do They Compare to Other Treatments?
Bisphosphonates aren’t the only option. Denosumab (Prolia) is a monthly injection that works differently-it blocks a protein that activates osteoclasts. It’s more potent than bisphosphonates at increasing bone density, but if you stop it, your bone loss can rebound fast, sometimes leading to multiple spinal fractures. That means you can’t just quit it. You have to switch to something else.
Then there’s teriparatide (Forteo), which is the opposite of a bisphosphonate. Instead of slowing bone loss, it actually builds new bone. It’s an injectable hormone that stimulates osteoblasts. It can raise bone density by up to 13% in 18 months. But it’s expensive-around $1,800 a month-and you can only use it for two years. After that, you usually switch to a bisphosphonate to maintain the gains.
Romosozumab (Evenity) is newer. It does both: builds bone and slows breakdown. It’s powerful-reducing vertebral fractures by 73% in trials. But it carries a warning about heart attack risk. So it’s not for people with heart disease.
Here’s the bottom line: bisphosphonates still make up about 65% of all osteoporosis prescriptions in the U.S. Why? They’re proven, they’re safe for most people, and they’re cheap. Generic alendronate costs as little as $20 a month. That’s why they remain the first choice for most patients.
Who Should Be Tested-and How
You don’t need to wait for a fracture to get tested. If you’re a woman over 65, or a man over 70, a bone density scan (DXA) is recommended. Younger people with risk factors-like a family history of hip fractures, long-term steroid use, smoking, or low body weight-should also get checked. The test is quick, painless, and uses very little radiation.
Doctors also use the FRAX tool, which calculates your 10-year risk of a major fracture based on age, sex, weight, history of fractures, smoking, alcohol use, and other factors. If your risk is above 20% for any major fracture or above 3% for a hip fracture, treatment is usually recommended. That’s often where bisphosphonates come in.
What Patients Really Say
Real people have real experiences. On patient forums, you’ll hear both sides. One woman wrote, “I broke my wrist at 62. My doctor put me on alendronate. After two years, my bone density improved. I haven’t had another fracture.” Another man said, “I couldn’t take the pill because it burned my throat. I switched to the yearly IV. No more pain. No more stress.”
But others say: “I gave up on the pills because I forgot every week.” Or, “I was on it for six years, then stopped. Now I’m scared I’ll break something.” These stories highlight a key truth: adherence matters. If you don’t take the medicine as directed, it won’t work. And if you stop without a plan, you might be worse off.
What Comes Next?
The future of osteoporosis treatment is personal. We’re moving away from one-size-fits-all. Now, doctors look at your fracture risk, your age, your other health conditions, and even your dental history. Some patients will stay on bisphosphonates for life. Others will switch after a few years. Some will need anabolic drugs. The goal isn’t just to slow bone loss-it’s to keep you mobile, independent, and fracture-free.
Research is also looking at better ways to monitor treatment. Right now, we rely on bone density scans every one to two years. But scientists are testing new blood and urine markers that might tell us sooner if the drug is working. And there’s ongoing work on longer-acting formulations that could mean fewer doses.
For now, bisphosphonates remain the foundation. They’re not flashy, but they’ve saved millions from fractures. The key is using them right-starting at the right time, taking them correctly, and knowing when to pause. Because with osteoporosis, the best treatment isn’t the newest drug. It’s the one you’ll actually take.
Can bisphosphonates rebuild bone or just stop it from breaking down?
Bisphosphonates primarily slow down bone loss by targeting osteoclasts, the cells that break down bone. They don’t directly build new bone. However, by reducing bone breakdown, they allow the body’s natural bone-forming cells (osteoblasts) to gradually rebuild bone structure over time. This leads to a net gain in bone density-typically 5% to 10% over three years-but it’s not the same as actively stimulating bone growth like anabolic drugs (e.g., teriparatide) do.
Why do I have to stay upright after taking an oral bisphosphonate?
Oral bisphosphonates can irritate the esophagus if they don’t move quickly into the stomach. Staying upright (sitting or standing) for at least 30 minutes helps the pill reach your stomach faster and reduces the chance of it lingering in the esophagus. This prevents inflammation, ulcers, or even esophageal damage. You also shouldn’t eat, drink, or take other medications during this time-only plain water.
What’s a drug holiday, and why is it recommended?
A drug holiday means temporarily stopping bisphosphonate treatment after 3 to 5 years, especially if your fracture risk has lowered and your bone density has improved. Bisphosphonates stay in your bones for years, so their effects continue even after you stop. This break reduces the risk of rare side effects like atypical femur fractures or osteonecrosis of the jaw. Your doctor will monitor your bone density and overall risk before deciding whether to restart the medication.
Are bisphosphonates safe for people with kidney problems?
Not all bisphosphonates are safe for people with kidney issues. Oral bisphosphonates generally require a creatinine clearance of at least 30-35 mL/min. Zoledronic acid, the IV form, needs at least 35 mL/min. If kidney function is below these levels, the drug can build up in the body and cause harm. Your doctor will check your kidney function before prescribing any bisphosphonate and may choose a different treatment if your kidneys aren’t functioning well enough.
Can I take calcium and vitamin D with bisphosphonates?
Yes, and you should. Calcium and vitamin D are essential for bone health, and bisphosphonates work best when you have enough of them. But timing matters. You should take calcium and vitamin D supplements at least 30 to 60 minutes after taking your bisphosphonate. Taking them together can interfere with absorption, making the medication less effective.
More Articles

Buy Cheap Generic Levitra Online - Safe Guide & Tips
Learn how to safely buy cheap generic Levitra online, verify legit pharmacies, compare prices and avoid counterfeit pills with our step‑by‑step guide.
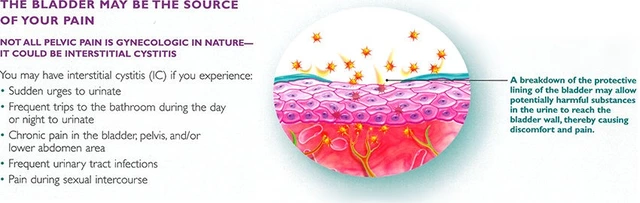
The Role of Diet in Preventing and Managing Cystitis
As a blogger, I cannot stress enough the importance of diet in preventing and managing cystitis. A balanced and healthy diet, rich in fresh fruits, vegetables, and whole grains, can help boost our immune system and prevent urinary tract infections. Drinking plenty of water and avoiding caffeine, alcohol, and spicy foods are crucial in managing cystitis symptoms. Including natural supplements like cranberry and D-mannose can also be helpful in preventing recurrent infections. Overall, our diet plays a significant role in maintaining a healthy urinary system and preventing cystitis.

