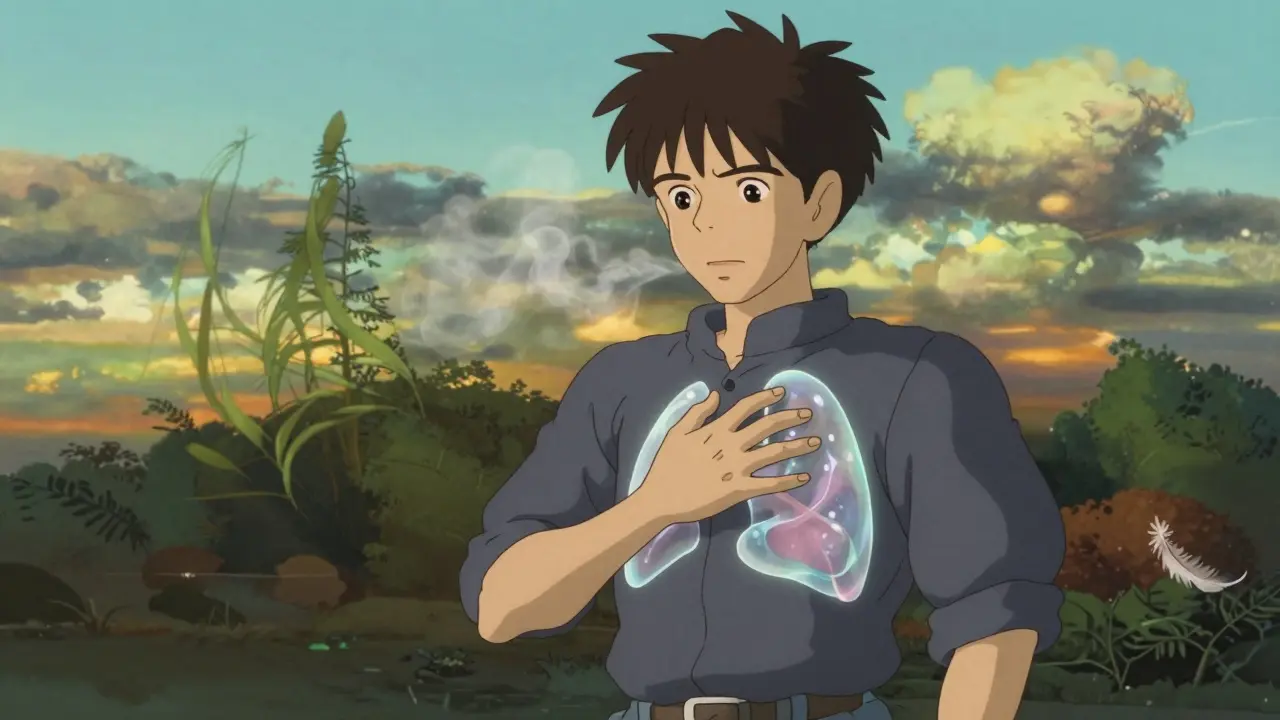
What Exactly Is a Pneumothorax?
A pneumothorax, or collapsed lung, happens when air leaks out of the lung and gets trapped between the lung and the chest wall. This air builds up pressure, pushing the lung down so it can’t expand properly when you breathe. It’s not just a minor inconvenience - it’s a medical emergency that can turn deadly fast if ignored.
You might think of your lungs like balloons inside a sealed box (your chest). Normally, the space around the lung is empty. But when air gets in there - from a rupture in the lung, a chest injury, or even spontaneously - it’s like poking a hole in the balloon. The lung collapses, and breathing becomes harder, sometimes impossible.
There are four main types: primary spontaneous (happens in healthy people, often tall, young men), secondary spontaneous (linked to diseases like COPD or cystic fibrosis), traumatic (from car crashes, stab wounds, or broken ribs), and iatrogenic (caused by medical procedures like biopsies or ventilator use). The risk isn’t equal for everyone. Smokers have a 22 times higher chance. Men are six times more likely than women. And if you’re over 70 inches tall, your risk jumps by more than three times.
How to Spot a Collapsed Lung - Symptoms You Can’t Ignore
The symptoms of pneumothorax are sharp, sudden, and hard to mistake. The most common sign is a stabbing chest pain on one side, usually worse when you take a deep breath or cough. It’s not a dull ache - it’s like a knife twisting with every inhale. About 92% of patients report this pain radiating to the same-side shoulder, a clue doctors look for right away.
Shortness of breath follows closely behind. In mild cases, you might only feel it when climbing stairs. But if more than 30% of your lung has collapsed, you’ll be gasping even at rest. Oxygen levels can drop below 90% - a red flag that your body isn’t getting enough air.
During a physical exam, doctors listen for two key signs: absent breath sounds on the affected side (present in nearly all confirmed cases) and hyperresonance - a drum-like sound when tapping the chest. These aren’t guesses. They’re measurable, repeatable findings backed by clinical studies.
When it turns into a tension pneumothorax, things get critical fast. This is when air keeps building up and pushes your heart and other organs sideways. Signs include a heart rate over 134 beats per minute, blood pressure dropping below 90, skin turning blue (cyanosis), and - though rare - the windpipe shifting away from the injured side. Tension pneumothorax kills within minutes if untreated. That’s why it’s diagnosed by symptoms, not waiting for an X-ray.
Emergency Care: What Happens in the ER
If you show up to the emergency room with suspected pneumothorax, time is everything. For tension pneumothorax, the rule is simple: act now, image later. If you’re struggling to breathe, your blood pressure is crashing, and your oxygen is below 90%, doctors won’t wait for a scan. They’ll stick a needle into your chest right away to release the trapped air. This is called needle decompression, and it’s life-saving. Studies show every 30-minute delay increases complication risk by 7.2%.
For non-emergency cases, the next step is imaging. A chest X-ray is the first test - it catches 85-94% of cases. But if you’re lying flat after a trauma (common in car accidents), the X-ray might miss it. That’s where ultrasound comes in. Emergency teams now use E-FAST scans, a quick ultrasound of the chest, which is 94% accurate and can be done in under a minute. In experienced hands, it’s faster and just as reliable as an X-ray.
Once diagnosed, treatment depends on size and symptoms. If the collapse is less than 15% and you’re breathing okay, you might just get oxygen and be sent home to watch and wait. Oxygen speeds up the body’s natural ability to reabsorb the air - from 1.25% per hour to over 4% per hour. But if you’re short of breath, or the collapse is bigger than 2 cm on the X-ray, you need a chest tube. That’s a tube inserted between your ribs to drain the air and let the lung re-expand.

When Surgery Is the Only Real Fix
Most first-time cases heal without surgery. But if it happens again - especially if you’re a smoker or have underlying lung disease - you’re at high risk for more episodes. After two collapses on the same side, the chance of a third jumps to 62%. That’s when doctors recommend surgery.
The gold standard is video-assisted thoracoscopic surgery (VATS). It’s minimally invasive: two small cuts, a camera, and instruments to remove the damaged part of the lung and seal the area. Success rates are 95% at one year. Recovery takes a few days in the hospital, and the cost in the U.S. is around $18,500 - but it cuts your recurrence risk from 40% down to just 3-5%.
For people who can’t have surgery, chemical pleurodesis is an option. A substance like talc is injected into the chest to create scar tissue that sticks the lung to the chest wall. It works in 88% of cases, but it’s painful - 25% of patients get severe pain right after. It’s not ideal, but it’s better than repeated collapses.
What Happens After You Leave the Hospital
Getting discharged doesn’t mean you’re out of the woods. Follow-up is crucial. You’ll need a chest X-ray in 4-6 weeks to make sure the lung fully re-expanded and no new air has leaked in. Studies show 8% of patients develop delayed problems if they skip this check-up.
Here’s what you must avoid:
- No flying for at least 2-3 weeks after recovery. Changes in cabin pressure can cause the lung to collapse again.
- No scuba diving unless you’ve had surgery. The risk of another collapse underwater is over 12% - and you won’t be able to surface if it happens.
- No smoking. Quitting cuts your recurrence risk by 77% in just one year. That’s not a suggestion - it’s medical necessity.
Patients who get clear, written instructions when they leave the hospital are 32% less likely to come back. That means knowing the warning signs: sudden sharp pain, blue lips, or being unable to speak in full sentences. If any of those happen, call emergency services immediately.

Who’s at Highest Risk - And Why It Matters
Not everyone has the same risk. If you’re a tall, thin male under 40 with no lung disease, you’re more likely to get a primary spontaneous pneumothorax. But if you’re a 70-year-old with COPD, your risk is far higher - and your chance of dying from it is 100 times greater.
Secondary pneumothorax (linked to lung disease) has a 16.2% one-year mortality rate. Primary cases? Just 0.16%. That’s not a small difference - it’s the difference between a scary scare and a life-threatening event.
That’s why doctors treat them differently. A young person with a small collapse might just go home. An older person with COPD and even a tiny air leak? They get a chest tube right away. Risk isn’t theoretical - it’s calculated, measured, and acted on.
Final Takeaway: Don’t Wait, Don’t Guess
Pneumothorax doesn’t always come with warning. It can strike someone who’s never had a problem before. The key is recognizing the signs early - sudden, sharp chest pain and trouble breathing. Don’t assume it’s a pulled muscle or heartburn. Don’t wait to see if it gets better. If you’re unsure, go to the ER. Every minute counts.
For those who’ve had it before, the message is clear: quit smoking, avoid high-risk activities, and get surgery if you’ve had two episodes. The numbers don’t lie - prevention saves lives.
9 Comments
Write a comment
More Articles

Rumalaya Gel vs Top Pain‑Relief Alternatives: Full Comparison 2025
A detailed 2025 guide compares Rumalaya gel with top pain‑relief alternatives, covering ingredients, price, safety, and when each product is best.

Epilepsy Surgery: Who Qualifies, What Risks Are Involved, and What Results to Expect
Epilepsy surgery offers real hope for those with drug-resistant seizures. Learn who qualifies, what risks are involved, and what outcomes you can realistically expect-backed by current medical guidelines and real patient data.

roger dalomba
December 26, 2025 AT 05:11So let me get this straight - if I’m tall, skinny, and breathe, I’m basically a walking time bomb? Thanks for the reassurance, doc. I’ll just go ahead and stop inhaling then.