Renal Antibiotic Dosing Calculator
Calculate creatinine clearance using the Cockcroft-Gault equation to determine appropriate antibiotic dosing for patients with kidney disease. Important: eGFR is not recommended for antibiotic dosing.
WARNING
Incorrect dosing increases risk of:
- Vancomycin: Hearing loss
- Penicillin: Seizures
- Aminoglycosides: Kidney damage
When someone has kidney disease, giving them the same antibiotic dose as a healthy person isn’t just risky-it can be deadly. Up to 60% of commonly used antibiotics are cleared by the kidneys. If those kidneys aren’t working right, the drugs build up. That’s when you see hearing loss from vancomycin, seizures from penicillin, or kidney damage from aminoglycosides. The fix isn’t stopping antibiotics-it’s adjusting the dose. And it’s not optional. In patients with kidney disease, wrong dosing increases death risk by nearly 30% in pneumonia and nearly 20% in urinary infections.
Why Kidney Function Changes Everything
Your kidneys don’t just make urine. They filter toxins, including antibiotics, out of your blood. When kidney function drops, those drugs stay in your body longer. That sounds harmless until you realize: antibiotics aren’t like painkillers. They’re designed to kill bacteria at specific concentrations. Too little? The infection doesn’t clear. Too much? You poison yourself. The key number doctors use is creatinine clearance (CrCl). It’s not a direct measurement-it’s calculated. The most trusted formula is the Cockcroft-Gault equation. You plug in age, weight, sex, and serum creatinine. For men: CrCl = [(140 - age) × weight (kg)] / [72 × serum creatinine]. For women, multiply that result by 0.85. It’s old, but it’s still the gold standard. Why? Because it accounts for muscle mass. eGFR, which is more common in general medicine, doesn’t. And in antibiotic dosing, that difference matters. Kidney function is split into clear buckets:- Normal: CrCl >50 mL/min
- Mild impairment: CrCl 31-50 mL/min
- Moderate impairment: CrCl 10-30 mL/min
- Severe or on dialysis: CrCl <10 mL/min
Which Antibiotics Need Dose Adjustments?
Not all antibiotics behave the same. Some are like water-they pass through kidneys easily and need big changes. Others are mostly broken down by the liver and barely touch the kidneys. The rule of thumb: if the drug’s label says “renal adjustment required,” it’s not a suggestion. It’s a warning. Take ampicillin/sulbactam. Standard dose: 2 grams every 6 hours. For CrCl 15-29 mL/min? Drop to 2 grams every 12 hours. For CrCl under 15? Only 2 grams every 24 hours. Go too high? You risk brain toxicity. Too low? The infection comes back. Cefazolin is different. It’s forgiving. Even in severe kidney disease, you can give 500 mg to 1 gram every 12 to 24 hours. That’s because it has a wide therapeutic index-there’s a big safety gap between effective and toxic doses. But here’s the trap: doctors often reduce it too much. In acute kidney injury, underdosing increases treatment failure by 34%. Then there’s clarithromycin. One guideline says reduce to 500 mg daily if CrCl is under 30. Another says keep it at 500 mg daily even if CrCl is under 50. That kind of inconsistency is why 41% of hospital pharmacists say they struggle to choose the right dose. And don’t forget vancomycin. It’s a classic. You need a loading dose-25-30 mg/kg-even in kidney failure. Then you hold back on maintenance. But if you skip the loading dose, you delay killing the bacteria. That’s why guidelines say: load first, then adjust.The Big Problem: Acute vs. Chronic Kidney Disease
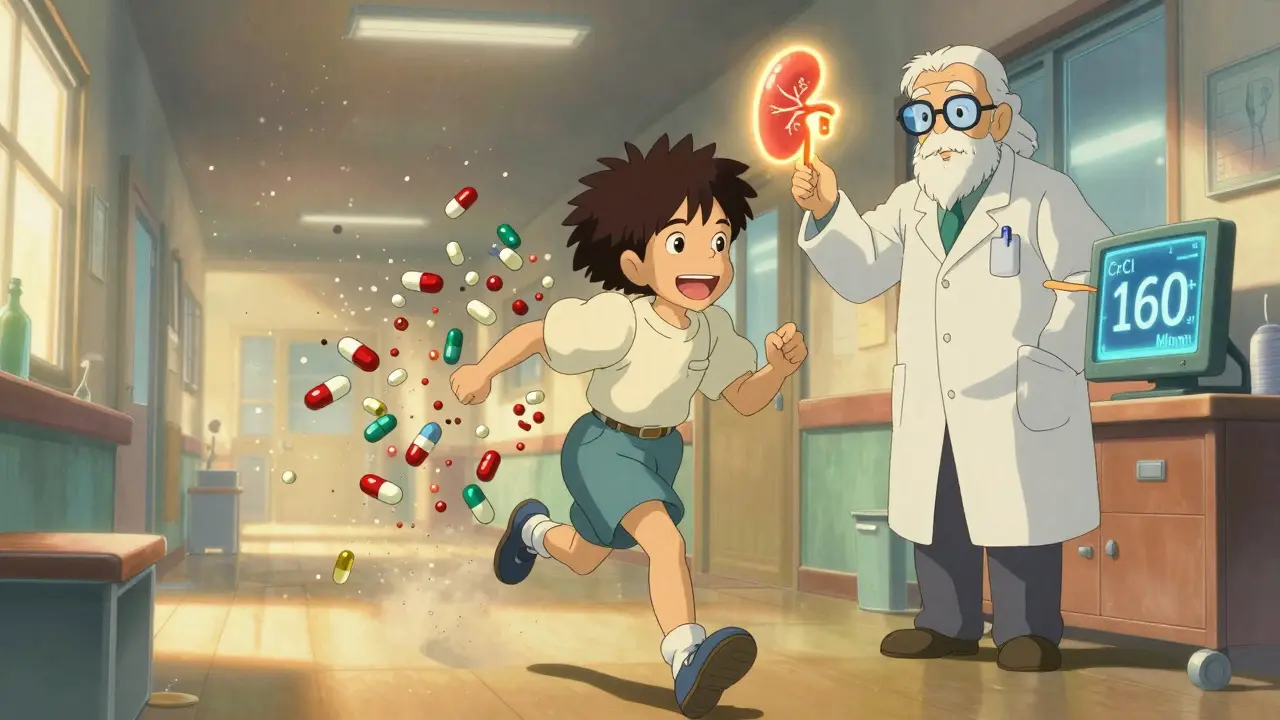
Most dosing guidelines were built for people with stable chronic kidney disease (CKD). But what about someone who just had a heart attack and now has acute kidney injury (AKI)? Their CrCl might be 15 today, but 60 tomorrow. If you reduce their antibiotic dose based on today’s number, you might be underdosing them during the critical first 48 hours. A 2019 review found that 57% of AKI cases resolve within two days. Yet, we treat them like they have permanent kidney failure. That’s dangerous. Studies show that unnecessary dose reductions in AKI lead to treatment failure in 34% of cases. Meanwhile, if you don’t reduce the dose when CrCl drops below 10, you risk toxicity. The real issue? Guidelines don’t distinguish between these two. They treat all low CrCl the same. That’s why experts like Dr. Jason Roberts say we need to rethink dosing in the first 72 hours of infection. For antibiotics with wide therapeutic indices-like cefazolin, amoxicillin, or ceftriaxone-hold off on reducing the dose until you’re sure the kidney injury is lasting.What About Augmented Renal Clearance?
It sounds like a good thing-your kidneys are working overtime. But in young trauma patients, sepsis survivors, or athletes, CrCl can shoot past 130 mL/min. That’s called augmented renal clearance. And it’s a hidden problem. If you give a standard dose of piperacillin/tazobactam to someone with CrCl of 160, the drug gets flushed out before it can kill bacteria. That’s why UNMC recommends 2 grams every 4 hours in these cases. Most other guidelines don’t even mention it. But if you don’t adjust, the infection doesn’t respond. And that’s how you end up with treatment failure-even in healthy-looking young patients.How to Get It Right in Real Life
Knowing the rules isn’t enough. Applying them is harder. A 2023 survey of 1,247 clinicians found that 63% couldn’t calculate CrCl correctly. Many forgot to use ideal body weight in obese patients. Others used serum creatinine without checking if it was from a recent blood test. One wrong number throws off the whole dose. Here’s how to fix it:- Use institutional protocols. 72% of academic hospitals pick one guideline-usually KDIGO-and stick to it. No more confusion between UNMC and Northwestern Medicine.
- Turn on EHR alerts. 89% of U.S. hospitals now have electronic warnings when a drug is ordered and CrCl is low. These alerts cut errors by 40%.
- Ask the pharmacist. Pharmacist-led dosing teams reduce antibiotic-related harm by 37%. They catch the missed loading dose, the wrong weight, the outdated formula.
- Check oral antibiotics too. Ciprofloxacin is often forgotten. Standard dose: 500 mg every 12 hours. For CrCl 10-30? Cut it to 250 mg every 12 hours. Miss this, and you’re underdosing.
The Future: AI, Monitoring, and Better Guidelines
The field is changing fast. The FDA now requires renal dosing studies for every new antibiotic since 2018. The European Medicines Agency does the same since 2020. Why? Because 32% of trial participants have some kidney impairment-and if you don’t test dosing in them, you don’t know if the drug works. Therapeutic drug monitoring (TDM) is growing. Instead of guessing the dose, you measure the drug level in the blood. Right now, only 38% of academic hospitals do it. By 2027, that could jump to 65%. For drugs like vancomycin and aminoglycosides, it’s already standard. Some hospitals are testing AI tools that auto-calculate CrCl, check for drug interactions, and suggest doses based on real-time lab values. Pilot programs are running in 17% of U.S. teaching hospitals. And the biggest shift? KDIGO’s 2023 update will finally separate acute from chronic kidney disease in its dosing advice. That’s huge. Because for too long, we’ve been treating temporary kidney injury like permanent damage.Bottom Line: Dose Smart, Not Just Less
Renal dosing isn’t about giving smaller pills. It’s about matching the drug to the patient’s kidney function-whether that’s low, high, or changing fast. The goal isn’t just to avoid toxicity. It’s to make sure the antibiotic works. Use Cockcroft-Gault. Know your antibiotics. Don’t reduce doses too early in acute injury. Don’t forget loading doses. Use alerts. Trust your pharmacist. And remember: if a patient’s kidney function changes, the dose should too. This isn’t just a pharmacy problem. It’s a patient safety issue. And in kidney disease, getting it right saves lives.14 Comments
Write a comment
More Articles
Insulin Allergies: How to Spot and Handle Injection Reactions
Insulin allergies are rare but serious. Learn how to spot the signs - from itchy bumps to life-threatening reactions - and what to do if you react to your insulin injection.



Kunal Majumder
January 10, 2026 AT 08:33Yo, this is gold. I work in a rural clinic in India and we don’t always have fancy lab results. But knowing CrCl matters? Life-saving. I’ve seen guys on vancomycin turn deaf after a week because someone just dosed by weight. Not cool.