
When we talk about senior oral health prophylaxis is a set of preventive practices designed to keep the teeth, gums, and mouth tissues healthy as people age, the aim is to avoid painful problems like gum disease, cavities, and tooth loss.
Key Takeaways
- Age‑related changes require a gentler, more thorough daily routine.
- Fluoride, interdental cleaning, and saliva‑boosting strategies are essential.
- Regular dental check‑ups every six months can catch issues early.
- Choosing the right tools - soft‑bristle brush, water floss, or denture cleanser - makes a big difference.
- Nutrition, medication management, and hydration all impact oral health.
How Aging Affects the Mouth
Older adults often experience dental plaque a sticky film of bacteria that forms on teeth and along the gum line more quickly because of reduced saliva flow, slower gum tissue regeneration, and sometimes limited dexterity. gum disease also known as periodontitis, is an infection that damages the soft tissue and bone supporting the teeth becomes a leading cause of tooth loss after 65. Medications commonly prescribed for blood pressure, depression, or allergies can cause dry mouth a condition called xerostomia that diminishes the mouth's natural cleaning action, increasing the risk of cavities and oral infections.
For denture wearers, changes in the shape of the jawbone can affect fit, leading to irritation or reduced chewing efficiency. Understanding these shifts is the first step toward a proactive care plan.
Building a Daily Prophylactic Routine
A solid routine doesn’t have to be complicated, but it should address the unique needs of seniors.
- Brush gently twice a day. Use a soft‑bristle toothbrush designed to clean without irritating sensitive gums and a pea‑size amount of fluoride toothpaste provides extra protection against decay, especially important when saliva flow is low. Hold the brush at a 45‑degree angle and use short, circular motions.
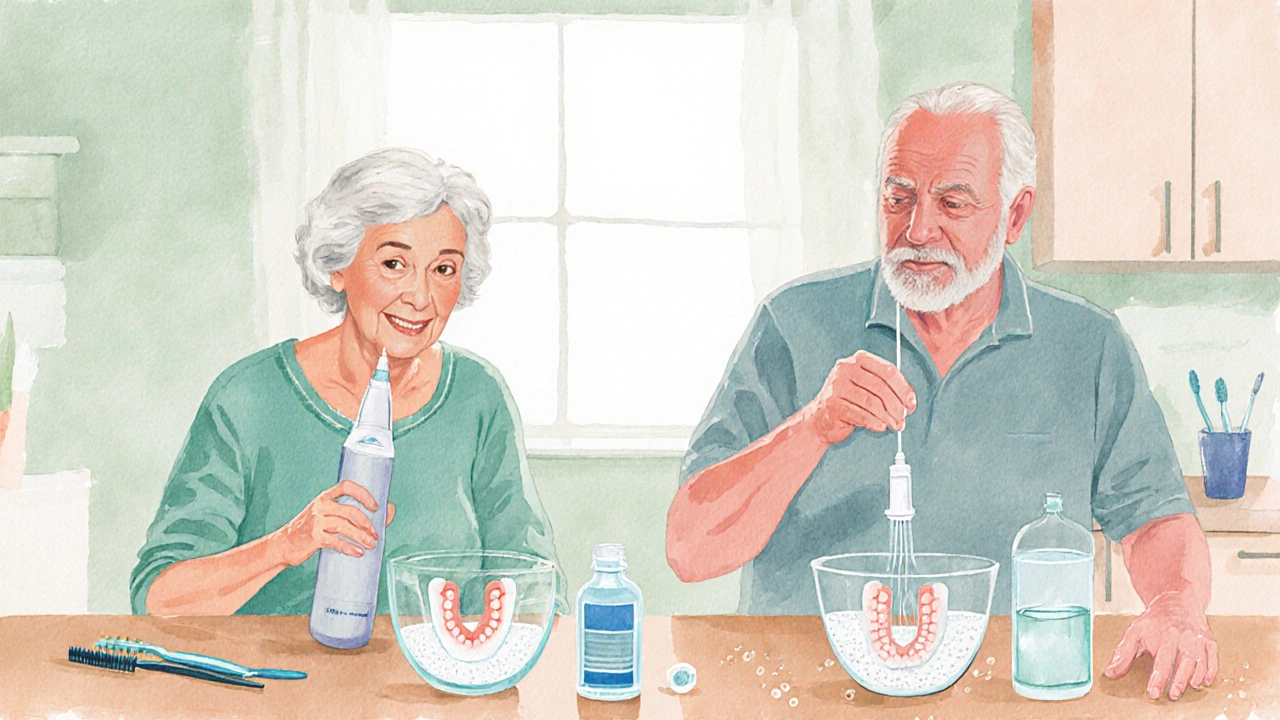
- Clean between teeth. Traditional floss can be tough on fragile gums. Many seniors find interdental brushes small, flexible brushes that fit between teeth and around dental work or water flossers easier to handle. Aim for once a day.
- Rinse with a therapeutic mouthwash. Choose an alcohol‑free rinse containing chlorhexidine or essential oils to lower bacterial load without drying out the mouth.
- Moisturize the mouth. If you suffer from dry mouth, sip water frequently, chew sugar‑free gum, or use a saliva substitute a gel or spray that mimics natural saliva and eases discomfort after meals.
- Don’t forget dentures. Remove them nightly, brush with a denture‑specific cleanser, and soak them in a mild solution to prevent plaque buildup.
Addressing Common Age‑Related Oral Issues
Even with a solid routine, specific problems can pop up. Here’s how to tackle them.
- Dry mouth management. Besides frequent water intake, ask your doctor about adjusting medications that cause xerostomia. Over‑the‑counter saliva substitutes can provide temporary relief.
- Early gum disease. Look for red, swollen gums that bleed during brushing. A gentle professional cleaning and a targeted antimicrobial mouthwash can halt progression.
- Cavities on root surfaces. As gums recede, exposed root surfaces become vulnerable. Fluoride varnish applications during dental visits can protect these areas.
- Denture irritation. Ill‑fitting dentures can cause sore spots. Have them relined annually and use soft liners if needed.
Nutrition, Lifestyle, and Medications
What you eat and how you live directly affect oral health.
- Limit sugary snacks. Bacteria feed on sugars, producing acids that erode enamel. Choose fresh fruit, cheese, or nuts for a quick bite.
- Boost calcium and vitamin D. Strong teeth need mineral support. Dairy, leafy greens, fortified plant milks, and safe sunlight exposure help maintain bone density in the jaw.
- Avoid tobacco and excessive alcohol. Both increase the risk of gum disease and oral cancers.
- Check medication side effects. Many prescription drugs list dry mouth as a side effect. Talk to your physician about alternatives or supportive measures.
Professional Care: When and Why to Visit the Dentist
Self‑care is vital, but you still need a professional eye.
- Routine check‑ups every six months. Even if everything feels fine, a dentist can spot early decay, gum inflammation, or denture wear.
- Professional cleanings. Scaling removes hardened plaque (tartar) that home brushing can’t reach.
- Fluoride treatments. In‑office application of high‑strength fluoride strengthens enamel, especially useful for those with dry mouth.
- Radiographs. X‑rays reveal hidden decay and bone loss beneath the gum line.

Choosing the Right Products - A Quick Comparison
| Product | Key Feature | Best For | Price Range (AU$) |
|---|---|---|---|
| Soft‑Bristle Manual Toothbrush | Extra‑soft bristles, ergonomic handle | Gentle cleaning, limited dexterity | 3-8 |
| Electric Toothbrush with Pressure Sensor | Timers, gentle pulse, pressure feedback | Improved plaque removal, reduces over‑brushing | 50-150 |
| Interdental Brushes (Size0‑2) | Flexible heads, easy‑grip handle | Replacing floss, cleaning around implants | 8-20 (pack of 12) |
| Water Flosser (Low‑Pressure) | Adjustable stream, tip for braces | Users with arthritis or limited hand strength | 70-180 |
| Fluoride Mouthwash (Alcohol‑Free) | 10‑ppm fluoride, no burning sensation | Dry‑mouth sufferers, daily use | 12-25 |
| Denture Cleanser Tablets | Effervescent, removes stains, anti‑plaque | Full‑time denture wearers | 4-10 (30‑tablet pack) |
Common Pitfalls & Pro Tips
Even the most careful seniors can slip into habits that undermine oral health. Spot the red flags and apply these fixes.
- Skipping night brushing because of fatigue - keep a travel‑size brush by the bedside for a quick swipe.
- Using a hard‑bristle brush - switch to soft or medium‑soft immediately to protect gum tissue.
- Rinsing with plain water after fluoride toothpaste - wait at least 30 minutes before eating or drinking to let fluoride work.
- Neglecting denture hygiene - a nightly soak prevents plaque and odor buildup.
- Forgetting to inform the dentist about new medications - updates help tailor preventive care.
Frequently Asked Questions
How often should I replace my toothbrush?
Every three months, or sooner if the bristles look frayed. Seniors with reduced saliva may need to change it a bit earlier to maintain optimal cleaning.
Is it safe to use a standard mouthwash if I have dry mouth?
Alcohol‑based mouthwashes can worsen dryness. Choose an alcohol‑free, fluoride‑enhanced rinse, or ask your dentist for a prescription antimicrobial rinse.
What signs indicate I need to see a dentist sooner than my regular check‑up?
Bleeding gums, persistent bad breath, sudden tooth sensitivity, loose dentures, or any sore that doesn’t heal within a week should trigger an early appointment.
Can I use regular floss if I have arthritis?
Traditional floss can be painful. Try floss picks, interdental brushes, or a water flosser with a low‑pressure setting for a gentler experience.
Do denture wearers need fluoride?
Yes. Even though dentures don’t have enamel, the underlying gums and any remaining natural teeth benefit from fluoride. A fluoride mouthwash or weekly varnish can help.
15 Comments
Write a comment
More Articles

Swollen Glands: Recognizing When to Seek Medical Attention
Swollen glands can be a worrying symptom and understanding when to seek medical attention is essential. This article explains the causes, symptoms, and when to be concerned about swollen glands. It provides practical tips and fresh insights into managing this common health issue. Reading this will help distinguish between minor and serious cases.


Bryan Kopp
October 9, 2025 AT 15:50Keeping a soft brush handy and not over‑brushing can actually keep the gums happier.