
Medication Constipation Risk Checker
Check if your medications are causing constipation and get personalized recommendations for managing it safely without stopping your prescriptions.
It’s not rare to start a new medication and suddenly find yourself stuck - not in traffic, but on the toilet. Constipation from medications is one of the most common, yet least talked about, side effects. You’re taking your painkiller, antidepressant, or blood pressure pill exactly as prescribed, but your bowels have gone silent. You’re not lazy. You’re not eating wrong. Your body is reacting to the chemistry of the drug itself.
Why Your Pills Are Slowing You Down
Not all constipation is the same. When it’s caused by medicine, it’s not about lack of fiber or water. It’s about your gut nerves being put to sleep. Opioids like oxycodone or morphine bind to receptors in your intestines. These receptors normally help move food along. When they’re blocked, your gut slows down - sometimes by 40%. Fluid gets sucked out of your stool, turning it into hard, rock-like pellets. You might not even feel the urge to go. Anticholinergics - found in old-school allergy pills like diphenhydramine (Benadryl), some antidepressants, and even motion sickness patches - do something similar. They block a chemical called acetylcholine that tells your gut to contract. Without it, your intestines just sit there. Studies show up to 30% of people on these drugs get constipated. Calcium channel blockers, used for high blood pressure or chest pain, relax smooth muscle. That’s good for your arteries. Not so good for your colon. Drugs like verapamil can slow transit time by 20-25%. Diuretics? They dry you out. Less water in your system means less moisture in your stool. Iron supplements? They irritate the gut lining and mess with your good bacteria. Even some antipsychotics like clozapine can cause severe constipation - up to 35% slower movement. The scary part? Many people don’t realize this is a side effect of their meds. They think it’s just aging, or stress, or eating too much pasta. By the time they tell their doctor, they’ve been suffering for weeks.What Doesn’t Work (And Might Make It Worse)
If you’ve tried fiber supplements like Metamucil and it made things worse, you’re not alone. Bulk-forming laxatives are designed for people with slow digestion due to low fiber intake. But when your gut isn’t moving because of a drug, adding bulk is like throwing more logs on a fire that’s already out. It just sits there, swollen and painful. Studies show fiber can make medication-induced constipation worse in 20-30% of cases, especially with opioids. The stool gets bigger, but the muscles still won’t push. You end up bloated, crampy, and more frustrated than before. Same goes for just drinking more water alone. Yes, hydration helps. But if your gut isn’t moving, extra water won’t magically pull your stool out. You need something that wakes up your intestines - or pulls water into them.The Right Fix for the Right Drug
You can’t treat all medication constipation the same way. The solution depends on what’s causing it. Opioids: The gold standard is a class of drugs called PAMORAs - peripheral μ-opioid receptor antagonists. These are special because they block the opioid effect in your gut, but not in your brain. So your pain stays under control, but your bowels wake up. Methylnaltrexone (Relistor) and naloxegol (Movantik) work in as little as 4 hours. Clinical trials show 30-40% more bowel movements within a day. They’re not cheap - around $1,200 a month without insurance - but for many, they’re life-changing. If you’ve been on opioids for more than a few weeks, talk to your doctor about starting one of these early. Anticholinergics: If you’re taking diphenhydramine for sleep or allergies, switch to loratadine (Claritin) or cetirizine (Zyrtec). These newer antihistamines cause constipation in only 2-3% of users, compared to 15-20% with Benadryl. It’s a simple swap that can make a huge difference. Calcium Channel Blockers: Not all of them are equal. Amlodipine causes constipation in 5-7% of people. Verapamil? Up to 15%. If you’re on verapamil and struggling, ask if switching to amlodipine is an option. It’s the same blood pressure control, with fewer gut problems. General Approach: For most drug-induced constipation, the best first-line options are osmotic laxatives and stimulant laxatives. Polyethylene glycol (PEG 3350) draws water into the colon. It’s gentle, safe for long-term use, and doesn’t cause dependency. Sennosides (like Senokot) stimulate the gut muscles directly. Together, they work for 60-70% of people. Start with PEG 17g daily and add sennosides 17mg if needed. Don’t wait until you’re blocked to start them - begin on day one of your new medication.
What You Should Do Right Now
If you’re on any of these drugs, here’s your action plan:- Check your meds. Opioids, anticholinergics, calcium channel blockers, diuretics, and iron supplements are the top offenders.
- Don’t wait. If you’re starting a new medication that causes constipation, begin a laxative the same day. Waiting until you’re constipated means you’re already behind.
- Start with PEG and sennosides. One daily dose of PEG 3350 (17g) and one sennoside tablet (17mg) is a safe, effective combo for most people.
- Avoid fiber supplements. Unless your doctor says otherwise, skip psyllium or methylcellulose. They often make drug-related constipation worse.
- Drink 2-3 liters of water daily. Not because it will fix it alone - but because it helps the laxatives work better.
- Track your bowel movements. If you’re having fewer than three per week, or if you’re straining, feeling incomplete, or needing to manually assist, you’re constipated - even if you think it’s "normal."
Why So Many People Are Still Suffering
Here’s the truth: doctors aren’t always trained to think about this. A 2022 study in JAMA Internal Medicine found only 35-40% of primary care providers routinely recommend laxatives when prescribing opioids. Even worse, 65-75% of patients get no warning about constipation at all. Patients often feel embarrassed to bring it up. Or they assume it’s just part of getting older. Or they’re afraid the doctor will think they’re overreacting. But here’s what you need to know: constipation from meds isn’t a minor annoyance. It’s a reason people stop taking life-saving drugs. In cancer pain management, up to 20% of patients quit opioids because of constipation - even when their pain is still bad. That’s not just uncomfortable. It’s dangerous.Real Stories, Real Relief
One woman on Reddit, living with chronic back pain and on oxycodone for years, said she hadn’t had a normal bowel movement in eight months. She tried everything - prune juice, yoga, enemas. Nothing worked. Her doctor finally prescribed methylnaltrexone. Within 4 hours, she had her first unassisted bowel movement in over two years. "I cried," she wrote. "I didn’t realize how much I missed just going without thinking about it." A cancer patient on clozapine told her support group she was on three different laxatives daily and still not getting relief. After switching to a combination of PEG and sennosides - and cutting out fiber - she went from needing help every day to having regular, comfortable movements. "It’s the only thing that didn’t make me feel like a medical experiment," she said.
What’s Coming Next
Science is catching up. New treatments are in the works. One experimental therapy, SER-287, targets gut bacteria to restore normal movement. Early results show a 40-50% improvement in symptoms. Mayo Clinic is already using AI in their electronic records to flag patients at risk and auto-suggest prophylactic laxatives - cutting MIC cases by 30%. But right now, the best tool you have is knowledge. You don’t have to suffer because of your meds. You don’t have to choose between pain control and bowel function. There are solutions that work - if you know what to ask for.Frequently Asked Questions
Can I just take more fiber if I’m constipated from medication?
No. Fiber supplements like psyllium often make medication-induced constipation worse. These drugs slow gut movement, and fiber adds bulk without helping the muscles push. Instead of relieving constipation, it can cause bloating, cramps, and even blockages. Stick to osmotic laxatives like PEG or stimulants like sennosides.
How long should I wait before calling my doctor about constipation?
Don’t wait. If you’re on a medication known to cause constipation - like opioids, anticholinergics, or calcium channel blockers - start a laxative on day one. If you haven’t had a bowel movement in three days, or you’re straining hard, feeling full, or needing to use your fingers to help, contact your doctor. Early action prevents complications like fecal impaction.
Are over-the-counter laxatives safe for long-term use?
Osmotic laxatives like polyethylene glycol (PEG) are safe for long-term use and don’t cause dependency. Stimulant laxatives like sennosides are also safe for months if used correctly, but shouldn’t be the only solution for years. Avoid stimulants like senna for more than a year without medical supervision. Laxatives with phenolphthalein or cascara are banned in many countries - check your label.
Why is Relistor so expensive, and are there cheaper alternatives?
Relistor (methylnaltrexone) is expensive because it’s a specialized drug that only works in the gut. Generic alternatives don’t exist yet. But for many, PEG and sennosides work just as well - and cost under $10 a month. If those fail, talk to your doctor about patient assistance programs. Some manufacturers offer discounts or free trials for qualifying patients.
Can I stop my medication if constipation is too bad?
Never stop a prescribed medication without talking to your doctor. For some, like opioids for cancer pain or antipsychotics for severe mental illness, stopping suddenly can be dangerous. The goal isn’t to stop the drug - it’s to treat the side effect. There are effective, targeted treatments available. Ask your doctor about PAMORAs, switching medications, or adjusting your laxative plan.
What foods help with medication-induced constipation?
Food alone won’t fix it, but staying hydrated helps laxatives work. Drink 2-3 liters of water daily. Avoid excessive dairy and processed foods. Some people find prunes, kiwi, or chia seeds help mildly - but don’t rely on them. Focus on the right laxatives first, then use food as a gentle support.
What to Do Next
If you’re on a medication that causes constipation, don’t accept it as normal. Write down your meds. Note how often you’re going. If you’re below three bowel movements a week, or you’re straining, bloated, or feeling incomplete - you need help. Talk to your doctor. Say: "I’m on [medication name], and I think it’s causing constipation. What’s the best way to manage it without stopping the drug?" Bring this guide with you. Ask about PEG, sennosides, or PAMORAs. Most doctors haven’t been trained on this - but they’ll listen if you come prepared. You deserve to take your meds without suffering. There’s a solution that works. You just need to ask for it.13 Comments
Write a comment
More Articles

Constipation from Medications: How to Manage It Without Stopping Your Prescriptions
Constipation from medications is common but often ignored. Learn how to manage it safely without stopping your prescriptions, using proven laxatives, avoiding harmful fixes, and knowing when to ask for stronger help.
Favipiravir Patient Stories: Successes, Side Effects & Real‑World Challenges
Real patient stories reveal how Favipiravir helped COVID‑19 recovery, common side effects, and practical tips for safe use.
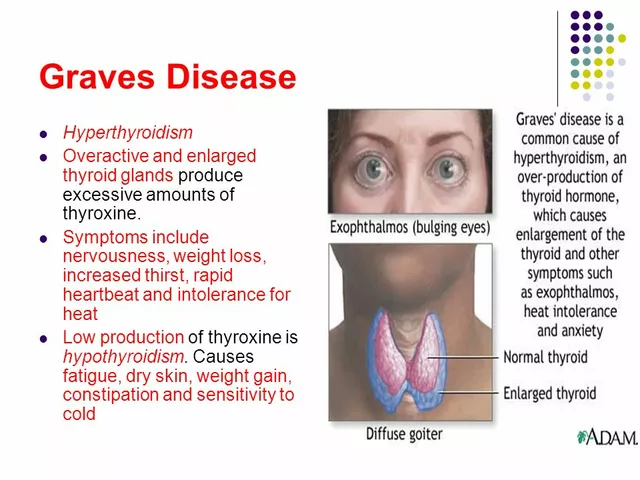
Diagnosing Graves' Disease: Signs, Symptoms, and Tests
I recently learned about Graves' disease, an autoimmune disorder that affects the thyroid gland. The common signs and symptoms include anxiety, weight loss, and a rapid heartbeat. It's important to be aware that some people might experience eye issues like bulging or discomfort. To diagnose this condition, doctors usually perform blood tests to measure thyroid hormone levels, and sometimes they might use imaging tests like ultrasounds. If you suspect you have Graves' disease, it's essential to consult with a healthcare professional to get a proper diagnosis and treatment plan.

Melissa Taylor
December 15, 2025 AT 05:05Thank you for writing this. I’ve been on oxycodone for five years and thought my constipation was just "part of aging." I started PEG last month and finally feel like myself again. No more dread before meals. No more guilt. This is life-changing.