Gluten Trigger Assessment for Crohn's Disease
Gluten Trigger Assessment
This assessment helps identify if gluten might be worsening your Crohn's disease symptoms. Answer the questions below to receive personalized guidance.
Answer the questions above to see your results.
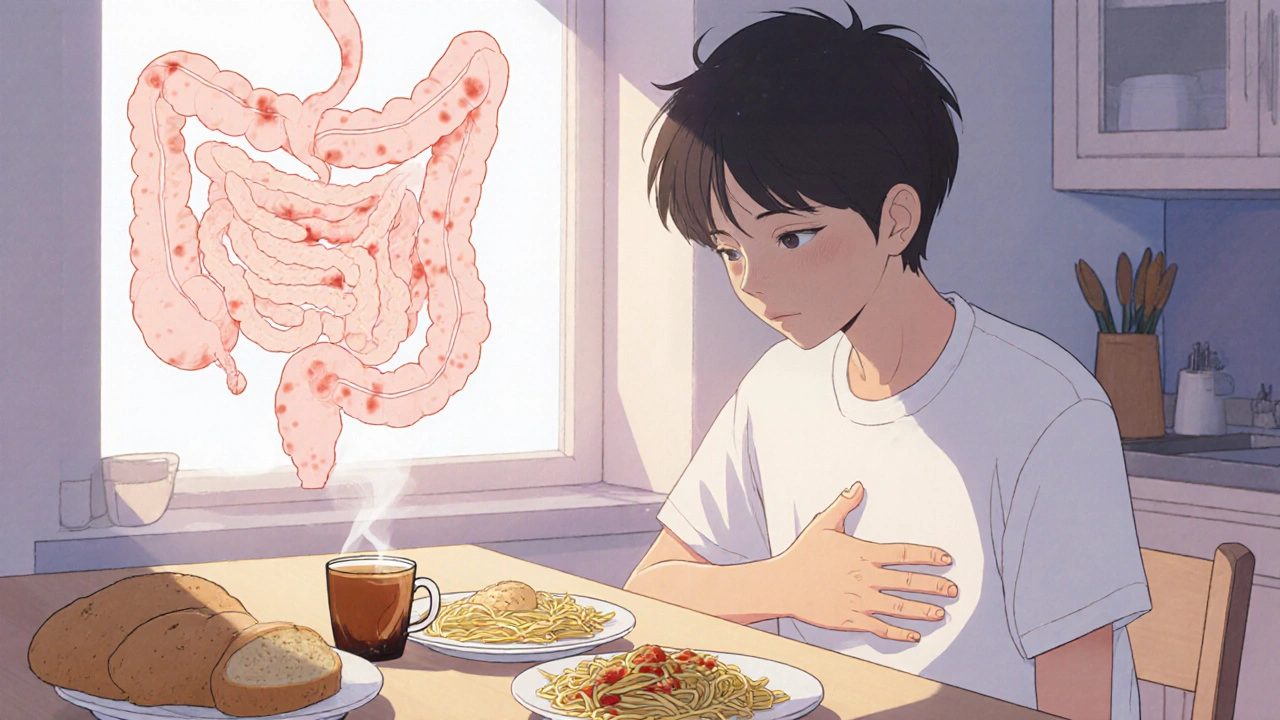
People with Crohn's disease is a chronic inflammatory bowel disease that can affect any part of the gastrointestinal tract. It causes abdominal pain, diarrhea, weight loss and fatigue. Many patients wonder whether gluten-a protein in wheat, barley and rye-might be quietly aggravating their condition. Recent studies show that a subset of Crohn's sufferers also react to gluten, blurring the line between classic celiac disease and non‑celiac gluten sensitivity.
Gluten intolerance is an umbrella term for adverse reactions to gluten that do not meet the full diagnostic criteria for celiac disease. Symptoms can range from bloating and stomach cramps to brain fog and joint pain. When these symptoms overlap with a Crohn's flare, pinpointing the exact trigger becomes a diagnostic puzzle.
Understanding Crohn's disease
Crohn's disease belongs to the broader category of Inflammatory bowel disease (IBD). It is driven by an autoimmune response that mistakenly attacks the lining of the gut. Genetic markers such as NOD2 and environmental factors-diet, smoking, stress-interact to fuel chronic inflammation. The disease can create ulcers, fistulas and strictures, often requiring medication, surgery, or both.
What exactly is gluten intolerance?<\/h2>
Gluten intolerance includes two main conditions: celiac disease, an autoimmune disorder linked to the HLA‑DQ2 or HLA‑DQ8 genes, and non‑celiac gluten sensitivity, which lacks the specific antibodies but still causes symptoms. Both involve increased intestinal permeability, sometimes called a “leaky gut,” allowing partially digested proteins to cross the gut wall and trigger inflammation.
Shared mechanisms: Why the two can overlap
Several biological pathways link Crohn's disease and gluten intolerance:
- Gut microbiome imbalance (dysbiosis): Both conditions show reduced diversity of beneficial bacteria such as Lactobacillus and increased pathogenic strains.
- Activation of immune cells like Th1 and Th17, which release cytokines (TNF‑α, IL‑17) that drive inflammation.
- Compromised intestinal barrier: Gluten peptides can bind to the zonulin receptor, opening tight junctions and worsening the permeability already present in Crohn's.
- Genetic predisposition: While NOD2 is classic for Crohn's, many patients also carry HLA‑DQ2/DQ8, making them susceptible to gluten‑related immune activation.
Red flags: Signs gluten might be fueling your Crohn's
Not every flare is gluten‑related, but watch for these patterns:
- Symptoms appear within 24‑48 hours after eating breads, pasta or processed foods containing wheat, barley or rye.
- Improvement occurs on a gluten‑free trial lasting at least two weeks, without other diet changes.
- Blood tests reveal elevated anti‑tTG antibodies or anti‑gliadin antibodies, even if celiac disease hasn’t been diagnosed.
- Concurrent extra‑intestinal issues-headaches, skin rashes (dermatitis herpetiformis‑like), or joint pain-that improve with gluten avoidance.

Testing the connection
To confirm whether gluten is a trigger, consider the following steps:
- Serology: Measure IgA anti‑tTG, anti‑endomysial and anti‑gliadin antibodies. A normal total IgA level is essential to avoid false negatives.
- Genetic testing: Detect HLA‑DQ2/DQ8. Absence makes celiac disease highly unlikely, but does not rule out non‑celiac sensitivity.
- Endoscopic biopsy: If serology is positive, an upper‑right‑quadrant duodenal biopsy can confirm villous atrophy.
- Gluten challenge: After a confirmed gluten‑free period, re‑introduce gluten under medical supervision and record symptom changes.
Dietary strategies for overlap patients
When you suspect gluten is a problem, a structured approach helps you stay nourished while testing:
- Elimination phase: Remove all sources of wheat, barley, rye, spelt and triticale for 4-6 weeks. Read labels carefully; many sauces and processed meats hide gluten.
- Low‑FODMAP boost: Combine gluten‑free eating with a low‑FODMAP diet to reduce fermentable carbs that also trigger bloating in Crohn's.
- Re‑introduction: Add back one gluten source at a time (e.g., gluten‑free oats, then sourdough‑style wheat) and monitor symptoms for a week each.
- Probiotic support: Strains like Bifidobacterium infantis and Saccharomyces boulardii can help restore gut balance during the trial.
When gluten isn’t the culprit
Even if gluten tests negative, other dietary triggers may mimic the same symptoms. Common offenders for Crohn's patients include:
- High‑fiber raw vegetables during active flare, which can irritate ulcerated lining.
- Artificial sweeteners (sorbitol, mannitol) that draw water into the colon.
- Dairy lactose, especially when the small intestine is inflamed.
Working with a dietitian who specializes in IBD can help you build a personalized plan that avoids unnecessary restrictions while ensuring adequate nutrition.
Comparison of Crohn's disease and gluten intolerance
| Aspect | Crohn's disease | Gluten intolerance (celiac & non‑celiac) |
|---|---|---|
| Primary cause | Autoimmune inflammation of any GI segment | Immune reaction to gluten peptides |
| Genetic markers | NOD2, ATG16L1 | HLA‑DQ2/DQ8 (celiac), no specific marker (NCGS) |
| Typical symptoms | Abdominal pain, diarrhoea, weight loss, fistulas | Bloating, diarrhoea/constipation, skin rash, fatigue |
| Diagnostic tests | Endoscopy, imaging, labs (CRP, fecal calprotectin) | Serology (anti‑tTG, anti‑gliadin), biopsy (celiac) |
| Treatment focus | Immunosuppressants, biologics, surgery | Strict gluten‑free diet (celiac) or gluten reduction (NCGS) |
| Overlap potential | Increased intestinal permeability can amplify gluten reaction | Gluten can worsen existing inflammation in Crohn's |
Practical checklist before going gluten‑free
- Consult your gastroenterologist to rule out active infection or strictures.
- Get baseline serology and, if indicated, a small‑bowel biopsy.
- Document your current diet and symptom log for at least two weeks.
- Prepare a gluten‑free pantry: rice, quinoa, certified gluten‑free oats, fresh fruits, lean proteins.
- Plan regular follow‑up appointments to reassess labs and disease activity.
Bottom line
While not everyone with Crohn's disease needs to avoid gluten, a noticeable pattern of symptoms after wheat‑based meals deserves attention. A systematic elimination, proper testing, and professional guidance can reveal whether gluten is a hidden aggravator. By tailoring your diet based on evidence-not fear-you can reduce flare‑ups, improve quality of life, and keep your gut on a more peaceful track.
Can a gluten‑free diet cure Crohn's disease?<\/h3>
No. Gluten‑free eating can soothe symptoms for some patients, but Crohn's is a complex autoimmune condition that usually requires medication and sometimes surgery. Diet is a supportive tool, not a cure.<\/p>
No. Gluten‑free eating can soothe symptoms for some patients, but Crohn's is a complex autoimmune condition that usually requires medication and sometimes surgery. Diet is a supportive tool, not a cure.<\/p>
How long should I stay gluten‑free before judging its effect?<\/h3>
A minimum of four weeks is recommended. This period allows gut healing and stabilises inflammation, making it easier to see real changes.<\/p>
A minimum of four weeks is recommended. This period allows gut healing and stabilises inflammation, making it easier to see real changes.<\/p>
Do I need a professional to test for gluten sensitivity?<\/h3>
While at‑home antibody kits exist, a gastroenterologist can interpret results in the context of Crohn's activity, order confirmatory biopsies, and ensure you aren’t missing other triggers.<\/p>
While at‑home antibody kits exist, a gastroenterologist can interpret results in the context of Crohn's activity, order confirmatory biopsies, and ensure you aren’t missing other triggers.<\/p>
Is it safe to take probiotics while on a gluten‑free trial?<\/h3>
Yes. Certain probiotic strains support gut barrier function and may reduce inflammation. Choose a product with clinically studied strains like Bifidobacterium infantis.<\/p>
Yes. Certain probiotic strains support gut barrier function and may reduce inflammation. Choose a product with clinically studied strains like Bifidobacterium infantis.<\/p>
What other foods commonly hide gluten?<\/h3>
Soy sauce, marinades, processed meats, soups, salad dressings and some spice mixes often contain wheat‑derived thickeners. Look for labels that say ‘gluten‑free’ or check the ingredient list for wheat, barley, rye, malt or triticale.<\/p>
Soy sauce, marinades, processed meats, soups, salad dressings and some spice mixes often contain wheat‑derived thickeners. Look for labels that say ‘gluten‑free’ or check the ingredient list for wheat, barley, rye, malt or triticale.<\/p>
13 Comments
Write a comment
More Articles

Top 7 Alternatives to Finasteride in 2025: What's Right for You?
Exploring the top alternatives to Finasteride in 2025 offers insights for those seeking different solutions for conditions like BPH and hair loss. With options like Tadalafil providing specific benefits and drawbacks, understanding how each treatment works can help guide personal health decisions. This article presents detailed comparisons to assist in finding the most suitable choice. Whether managing urinary symptoms or tackling hair loss, these alternatives offer varied paths to explore. Dive into the pros and cons to discover the best fit for your needs.

Antivirals: How Resistance Develops, Common Side Effects, and Real Ways to Stay on Track
Antivirals can stop viruses-but only if you take them right. Learn how resistance develops, what side effects to expect, and real strategies to stay on track with your treatment.

Safer Alternatives to Warfarin: New Anticoagulant Options and Bleeding Risk Data
Curious if there’s something safer than warfarin for blood thinning? This article explores the latest research on bleeding risks and antidotes for the new class of anticoagulants. You’ll see clear comparisons, practical tips, and what to look for if you or a loved one may need a switch. Want peace of mind about managing your blood thinner? Read on for real-world data, not just theory. We even dig into alternatives and how to talk to your doctor about making the change.

Caleb Clark
October 22, 2025 AT 14:56Hey folks, I just wanted to share some upbeat thoughts about tackling that confusing overlap between Crohn's and gluten issues!
First off, remember that your gut is a resilient organ, even when it feels like it's constantly under attack.
Start by logging every bite and symptom – the data will become your best ally.
Don't get discouraged if you see a flare after a bagel; that's a clue, not a verdict.
Try a 4‑week gluten‑free trial while keeping your meds stable, and watch the pattern emerge.
Make sure you’re still getting enough protein – think chicken, fish, and eggs, not just rice cakes.
Probiotic supplements can be a game‑changer, especially those with Bifidobacterium infantis which help seal the leaky gut.
Drink plenty of water; hydration supports mucosal healing.
When you feel a twinge after a pizza, note the timing – 24‑48 hours is a typical window for gluten‑related reactions.
Stay in close contact with your gastroenterologist, share your logs, and ask for serology tests if you suspect gluten antibodies.
Remember, a gluten‑free diet is a tool, not a cure, so keep your biologics or other meds as prescribed.
If you notice skin rashes or brain fog easing during the trial, that’s another data point confirming the link.
Don't let the fear of restrictions overwhelm you; there are tasty gluten‑free alternatives like quinoa, buckwheat, and certified oats.
Keep an eye on fiber – some high‑fiber veggies can aggravate active inflammation, so balance is key.
Should a flare persist despite the diet, consider other triggers like dairy, high‑FODMAP foods, or stress.
Finally, celebrate small wins: a calmer stomach after a week, more energy, or clearer skin.
You're doing a great job navigating a complex condition, and every mindful step brings you closer to stability.