When you pick up a generic pill at the pharmacy, you might wonder: is this really the same as the brand-name version? The answer isn’t just yes - it’s backed by a rigorous, science-driven system designed to make sure every generic drug works exactly like its branded counterpart. The FDA doesn’t just approve generics because they’re cheaper. They approve them because they’ve passed tests that prove they’re therapeutically equivalent.
What Makes a Generic Drug the Same?
It’s not enough for a generic drug to have the same active ingredient. That’s just the starting point. The FDA requires two key things: pharmaceutical equivalence and bioequivalence.
Pharmaceutical equivalence means the generic has the same active ingredient, strength, dosage form (pill, liquid, injection), route of administration (oral, topical, etc.), and intended use as the brand-name drug. The label must say the same thing. Even the way it’s packaged and stored has to match.
But here’s where most people get confused: inactive ingredients can be different. That’s why your generic pill might be a different color or shape. It might have a different filler, dye, or preservative. These don’t affect how the drug works - only how it looks or tastes. The FDA allows this because it’s not about matching the brand’s packaging. It’s about matching its effect.
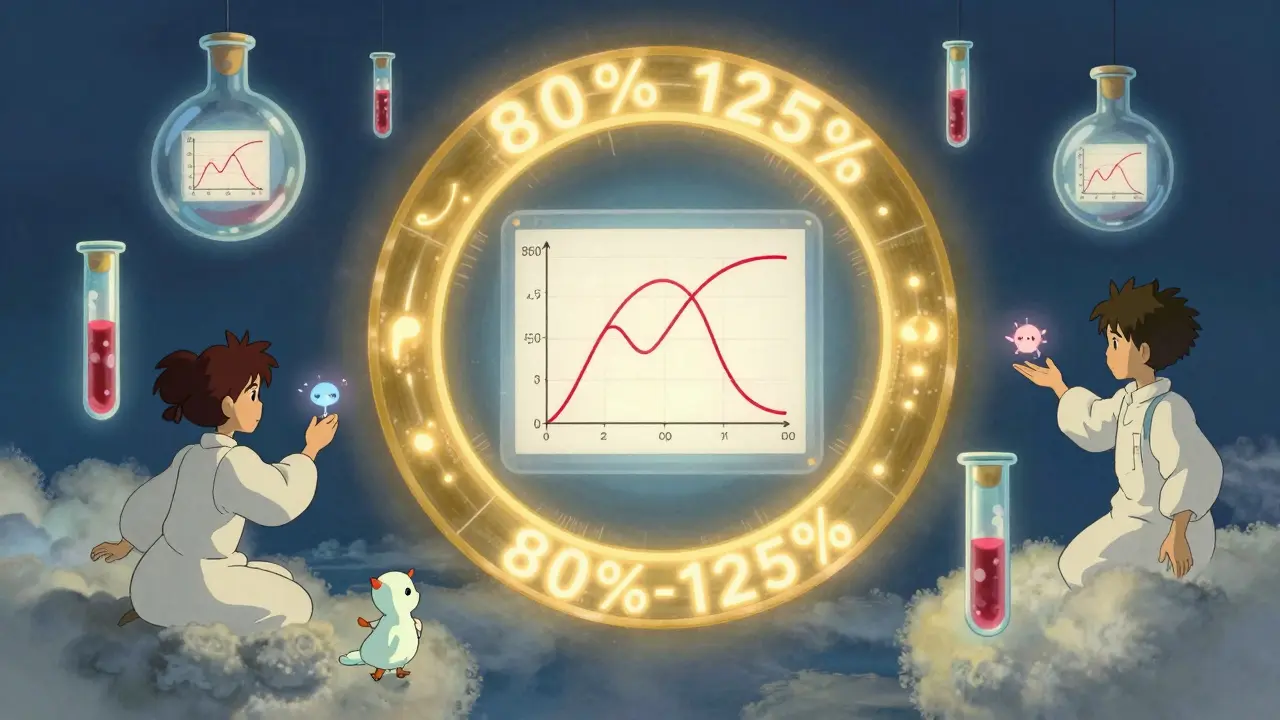
Bioequivalence is the real test. It means your body absorbs the generic drug at the same rate and to the same extent as the brand-name version. This isn’t guesswork. It’s measured with blood tests in healthy volunteers. The FDA requires that the 90% confidence interval for two key measurements - Cmax (peak concentration) and AUC (total absorption over time) - must fall between 80% and 125% of the brand-name drug. If it’s outside that range, the generic gets rejected.
The ANDA Process: How Generics Get Approved
Generic manufacturers don’t start from scratch. They file an Abbreviated New Drug Application, or ANDA. The word "abbreviated" doesn’t mean easy. It means they don’t need to repeat the expensive clinical trials the original company did. Instead, they focus on proving equivalence.
The ANDA must include:
- Proof of pharmaceutical equivalence
- Bioequivalence data from human studies
- Details on manufacturing processes
- Stability testing showing the drug won’t degrade before its expiration date
- Quality control methods for every batch
The FDA’s Office of Generic Drugs reviews each application. In 2022, they approved 892 original ANDAs and issued 478 complete response letters - meaning the application wasn’t ready. That’s a rejection rate of nearly 35%. Approval isn’t automatic. It’s earned.
Review timelines are tight. Under the Generic Drug User Fee Amendments (GDUFA), the FDA aims to review a complete ANDA in 10 months. That’s faster than many new drug approvals. Why? Because the system is funded by fees paid by generic manufacturers, which keeps the process moving.
Manufacturing: Same Rules, Same Facilities
Many people think generic drugs are made in sketchy factories. That’s not true. The FDA requires all manufacturers - brand or generic - to follow Current Good Manufacturing Practices (cGMP), codified in 21 CFR Parts 210 and 211. These rules cover everything: how raw materials are handled, how equipment is cleaned, how workers are trained, and how every batch is tested.
And here’s something surprising: about half of all generic drugs in the U.S. are made by the same companies that make brand-name drugs. They use the same facilities, the same equipment, and often the same quality control teams. The only difference? The label on the box.
The FDA inspects around 3,500 manufacturing sites every year - in the U.S. and overseas. No company gets a pass. If a plant fails inspection, the FDA can block shipments, delay approvals, or even shut down production.
Testing Complex Drugs: It’s Not All Pills
Not all generics are created equal - at least in how hard they are to test. For simple pills, blood levels are enough. But for inhalers, injectables, creams, or nasal sprays? It’s way more complicated.
The FDA has developed over 2,143 product-specific guidances for these complex drugs. These aren’t general rules. They’re detailed, drug-by-drug instructions on how to prove equivalence. For example, a generic inhaler doesn’t just need to deliver the same amount of drug. It needs to produce the same particle size, spray pattern, and lung deposition as the original. That requires advanced lab equipment and specialized testing.
In 2023, the FDA identified that 17% of complex generic products needed more than standard bioequivalence testing. Some required in vitro studies, pharmacodynamic measurements, or even small clinical trials. The agency invested $15.7 million in 2023 alone to improve testing methods for these harder-to-copy drugs.
Dr. Charles Ganley, former director of the FDA’s Office of Generic Drugs, pointed out in 2019 that for some complex products, "demonstrating equivalence requires more sophisticated testing than simple blood level measurements." That’s why the FDA holds public workshops and works with scientists worldwide to build better tools.
Why Generics Save Billions - And Why You Should Trust Them
Generic drugs made up over 90% of all prescriptions filled in the U.S. in 2023. Yet they accounted for only about 23% of total drug spending. In 2022 alone, they saved the healthcare system $37 billion.
Consumer Reports surveyed 1,200 U.S. adults in 2022. Eighty-nine percent were satisfied with their generic medications. Sixty-two percent said they chose generics specifically to save money.
But concerns linger. Some patients report issues - especially with drugs that have a narrow therapeutic index, like levothyroxine (for thyroid disease) or warfarin (a blood thinner). A 2021 JAMA study found that 12.3% of patients switching between different generic versions of levothyroxine needed dose adjustments due to changes in thyroid levels.
That doesn’t mean generics are unsafe. It means that for some drugs, even tiny differences in absorption can matter. The FDA tracks these reports closely and requires manufacturers to report any variability. In most cases, the differences are minor and don’t affect outcomes. But for patients on critical medications, sticking with one generic brand - or even the brand-name version - can be a smart choice.
Reddit’s r/pharmacy community had over 1,400 responses in a 2023 thread on generic vs. brand experiences. Eighty-three percent said they noticed no difference. Seventeen percent reported problems - mostly with seizure meds or blood thinners. The pattern? It wasn’t about generics being bad. It was about switching between different generic manufacturers too often.
What You Can Do
If you’re on a generic drug:
- Stick with the same manufacturer if it works for you. Switching between generics can sometimes cause issues.
- Ask your pharmacist if your generic is made by the same company as the brand. It might be.
- Don’t assume all generics are identical. Some have different inactive ingredients that might affect you.
- Monitor how you feel. If you notice changes in symptoms, energy, or side effects after switching, talk to your doctor.
The bottom line? FDA-approved generic drugs are not second-rate. They’re held to the same standards as brand-name drugs - and often made in the same places. The system works. It’s transparent. It’s tested. And it’s saved billions.
When you choose a generic, you’re not taking a risk. You’re choosing a proven, regulated, and cost-effective option that millions rely on every day.
Are generic drugs as effective as brand-name drugs?
Yes. The FDA requires generic drugs to have the same active ingredient, strength, dosage form, and route of administration as the brand-name version. They must also prove bioequivalence - meaning they’re absorbed into the body at the same rate and to the same extent. Over 90% of prescriptions in the U.S. are filled with generics, and studies show they work just as well.
Why do generic pills look different from brand-name pills?
Generic drugs can have different colors, shapes, or sizes because they use different inactive ingredients - like fillers, dyes, or coatings. These don’t affect how the drug works. The law only requires the active ingredient to be the same. The differences are cosmetic, not functional.
Can I trust generics made overseas?
Yes. The FDA inspects over 3,500 manufacturing facilities worldwide each year - including many in India and China. All facilities, whether domestic or foreign, must meet the same cGMP standards. About half of all generic drugs in the U.S. are made overseas, and the FDA’s track record shows they’re safe and effective.
Do generic drugs have the same side effects as brand-name drugs?
Yes, because they contain the same active ingredient, they cause the same side effects. However, some people may react differently to inactive ingredients - like dyes or preservatives - which can cause rare allergies or sensitivities. If you notice new symptoms after switching to a generic, talk to your doctor.
Are there any drugs where generics aren’t recommended?
The FDA considers all approved generics safe and effective. But for drugs with a narrow therapeutic index - like levothyroxine, warfarin, or certain seizure medications - even small changes in absorption can matter. Some doctors recommend sticking with one version (brand or generic) to avoid fluctuations. Always consult your doctor before switching.
How does the FDA ensure consistent quality across batches?
Every batch of a generic drug must be tested for identity, strength, purity, and quality before release. Manufacturers use validated methods and must meet compendial standards (like USP or EP). The FDA also conducts random inspections and tests samples from the market. If a batch fails, it’s destroyed. The FDA tracks quality trends and can shut down facilities that repeatedly fail.
What is bioequivalence testing, and how is it done?
Bioequivalence testing compares how the body absorbs a generic drug versus the brand-name drug. It’s done in 24-36 healthy volunteers who take both versions under controlled conditions. Blood samples are taken over time to measure peak concentration (Cmax) and total absorption (AUC). The results must fall within 80-125% of the brand-name drug’s values. This ensures the generic delivers the same therapeutic effect.
Why are some generics more expensive than others?
Price differences come from manufacturing costs, competition, and supply chain factors. A generic made by a brand-name company might cost more than one from a low-cost overseas manufacturer. But both meet the same FDA standards. The lowest price doesn’t mean lower quality - it usually just means less marketing or higher competition.
11 Comments
Write a comment
More Articles

Swollen Glands: Recognizing When to Seek Medical Attention
Swollen glands can be a worrying symptom and understanding when to seek medical attention is essential. This article explains the causes, symptoms, and when to be concerned about swollen glands. It provides practical tips and fresh insights into managing this common health issue. Reading this will help distinguish between minor and serious cases.


Simon Critchley
February 8, 2026 AT 06:49Let’s be real - the FDA’s bioequivalence window of 80-125% is basically letting generics slide if they’re half a standard deviation off the brand. 🤷♂️ I’ve seen generics that look like they were molded by a drunk intern. Cmax variability? More like Cmax roulette. And don’t get me started on the 35% rejection rate - that’s not rigor, that’s the FDA playing whack-a-mole with Chinese API suppliers.
Meanwhile, half the generics in your cabinet? Made by the same company as the brand. Same line. Same QA. Just a sticker swap. The system’s not broken - it’s just *brilliantly* gamed. 💥