
Gout Risk Calculator
This tool estimates your risk of a gout flare based on your dietary choices, hydration habits, and other lifestyle factors. Gout flares occur when uric acid crystals trigger an immune response in your joints.
Your Gout Flare Risk Assessment
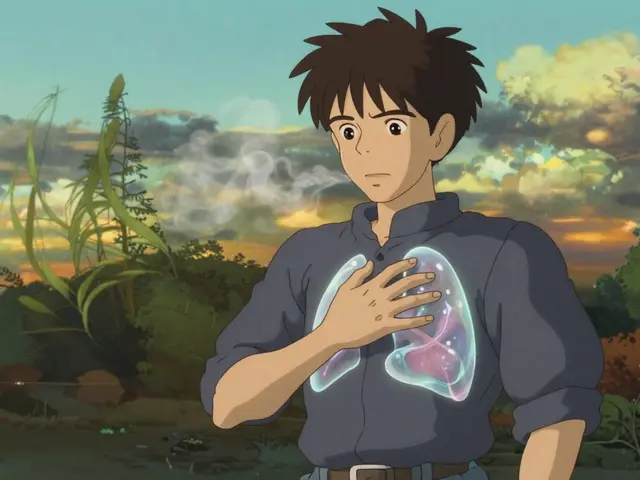
When Gout is a form of arthritis caused by high levels of uric acid that crystallize in joints, the immune system springs into action. This partnership between crystal deposits and immune cells explains why a flare feels like a sudden burn and why some people get repeated attacks.
Why the Immune System Gets Involved
Immune System the network of cells and molecules that defend the body against infection and injury isn’t just for colds. When monosodium urate (MSU) crystals settle in a joint, they act like tiny alarm bells. The body sees them as danger‑associated molecular patterns (DAMPs). Antigen‑presenting cells, especially macrophages, recognize these DAMPs through pattern‑recognition receptors and trigger an inflammatory cascade.
Key Immune Players in a Gout Flare
- Neutrophils - The first responders. They flood the joint within minutes, engulfing crystals and releasing enzymes that amplify pain.
- Cytokines - Signalling proteins like IL‑1β, IL‑6, and TNF‑α that fuel swelling and fever.
- NLRP3 Inflammasome - A protein complex inside macrophages that, once activated by urate crystals, chops pro‑IL‑1β into its active form. NLRP3 Inflammasome a multi‑protein platform that triggers inflammation when it detects cellular stress.
- IL‑1β - The master cytokine of gout. Blocking it can stop a flare in its tracks. IL‑1β a potent inflammatory molecule released after NLRP3 activation.
From Diet to Crystals: How Lifestyle Feeds the Fire
Not everyone with high uric acid gets gout. The tipping point is often diet. Foods rich in Purines nitrogen‑containing compounds that break down into uric acid-like red meat, organ meats, and certain seafood-raise blood urate levels. Alcohol, especially beer, interferes with uric acid excretion.
Hydration matters too. Low fluid intake reduces kidney clearance, allowing urate to accumulate and eventually crystallize.

Medical Treatments that Target the Immune Response
Traditional gout therapy focuses on pain relief, but newer drugs aim straight at the immune triggers.
- Colchicine - Disrupts microtubule formation, preventing neutrophil migration. Colchicine an anti‑inflammatory alkaloid taken during acute attacks.
- NSAIDs - Block COX enzymes, lowering prostaglandin‑mediated pain and swelling.
- Corticosteroids - Suppress multiple cytokine pathways, useful when NSAIDs or colchicine aren’t tolerated.
- IL‑1 Inhibitors - Drugs like canakinumab or anakinra neutralize IL‑1β, offering rapid relief for refractory flares.
Urate‑Lowering Therapy (ULT): The Long‑Term Defense
While anti‑inflammatories treat the flare, ULT addresses the root cause-excess uric acid. Here’s a quick look at the most common options.
| Drug | Mechanism | Typical Dose | Key Side Effects | Renal Considerations |
|---|---|---|---|---|
| Allopurinol Xanthine oxidase inhibitor that reduces uric acid production | Xanthine oxidase inhibition | 100-300 mg daily | Rash, hypersensitivity, liver enzymes | Requires dose adjustment if GFR <30 ml/min |
| Febuxostat | Selective xanthine oxidase inhibition | 40-80 mg daily | Cardiovascular warning, liver enzymes | Better tolerated in CKD than allopurinol |
| Probenecid | Increases renal uric acid excretion | 250-500 mg twice daily | Kidney stones, GI upset | Contra‑indicated if GFR <30 ml/min |
| Lesinurad (combined with a xanthine oxidase inhibitor) | URAT1 transporter inhibition | 200 mg daily | Kidney injury, liver enzymes | Use only with adequate hydration |
Starting ULT while an acute flare is ongoing can worsen symptoms. The usual strategy is: treat the flare first, then begin low‑dose ULT and titrate upward over weeks.

Managing Comorbidities: A Whole‑Body Approach
People with gout often have hypertension, obesity, or metabolic syndrome. These conditions raise urate production and impair kidney clearance. Tackling them simultaneously reduces flare frequency.
- Control blood pressure with ACE inhibitors or ARBs, which also improve uric acid excretion.
- Aim for a BMI <25 kg/m²; weight loss can lower serum urate by 0.5 mg/dL per 10 % weight loss.
- Screen for diabetes; high blood sugar can increase uric acid reabsorption.
Practical Checklist to Keep Gout in Check
- Track daily fluid intake; target >2 L water.
- Limit purine‑rich foods to <150 g per week.
- Avoid beer and sugary drinks.
- Maintain a regular exercise routine-30 minutes of moderate activity most days.
- Monitor serum urate every 2-3 months once on ULT.
- Keep a flare diary: note triggers, pain level, and meds used.
- Discuss IL‑1 inhibitor eligibility if flares occur >2 times/year despite optimal ULT.
Frequently Asked Questions
Can gout be cured?
There’s no permanent cure, but long‑term urate‑lowering therapy can keep serum urate below the crystallization threshold, effectively preventing new attacks for most people.
Why do some patients develop kidney stones?
Uric acid can precipitate in the urinary tract, especially when urine is acidic. Staying hydrated and, if needed, using alkalinizing agents reduces this risk.
Is colchicine safe for long‑term use?
Low‑dose colchicine (0.6 mg daily) is often used for prophylaxis and is generally safe, but it can cause diarrhea or muscle toxicity, especially in patients with kidney impairment.
How quickly does an IL‑1 inhibitor work?
Canakinumab can reduce pain within 24 hours; anakinra often shows improvement within a few hours, making them ideal for severe, refractory flares.
Should I stop ULT during a flare?
No. Stopping ULT can cause urate levels to bounce upward, potentially worsening the flare. Continue the daily dose and treat the flare with anti‑inflammatories.
Understanding how the immune system reacts to urate crystals transforms gout from a mysterious pain attack into a manageable condition. By pairing lifestyle tweaks with targeted medicines, most people can keep flares at bay and protect joint health for the long haul.
11 Comments
Write a comment
More Articles

Liability and Indemnification in Generic Transactions: What You Need to Know
Indemnification in commercial transactions shifts financial risk between parties through contract clauses. Learn how liability protection works, what triggers payouts, and how to negotiate fair terms to avoid costly surprises.


Bonnie Lin
October 23, 2025 AT 13:01Uric acid builds up when the body breaks down purines from foods like red meat and seafood. Staying well‑hydrated helps the kidneys flush excess urate and can lower flare risk. Reducing alcohol, especially beer, also supports long‑term control.