Most people with diabetes assume that if they’re having redness or swelling at their injection site, it’s just irritation from the needle. But what if it’s something more serious? Insulin allergy isn’t common - affecting only about 2.1% of insulin users - but when it happens, it can be dangerous if ignored. And here’s the catch: you might have been using insulin for years without a problem, then suddenly, your skin starts reacting. Or worse, you feel your throat tightening after an injection. This isn’t just a bad day. It’s your body telling you something’s wrong.
What Does an Insulin Allergy Actually Look Like?
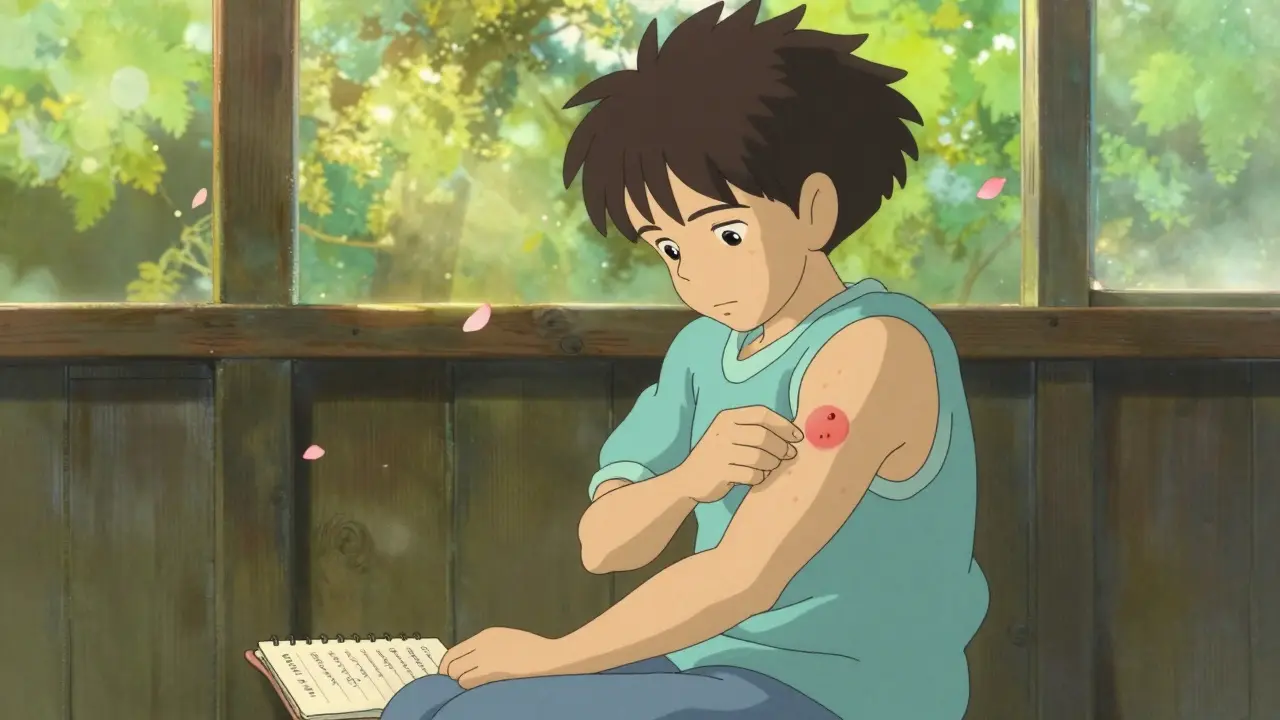
Not all reactions are the same. There are three main types, and knowing the difference can save your life.- Localized reactions happen right where you inject. Think red, itchy bumps, swelling, or hard lumps under the skin. These usually show up 30 minutes to 6 hours after your shot. They’re the most common - about 97% of all insulin allergy cases. Most fade within 1-2 days, but if they keep coming back, don’t brush them off.
- Systemic reactions are rare, affecting less than 0.1% of users, but they’re serious. These include hives, swelling of the lips or tongue, trouble breathing, dizziness, or a sudden drop in blood pressure. This is anaphylaxis. It can kill if you don’t act fast.
- Delayed reactions are the sneaky ones. You might feel joint pain, muscle aches, or notice bruising that doesn’t go away for weeks. These can appear even after 10 years of using insulin without issue. They’re not IgE-mediated like the others - they’re T-cell driven, meaning your immune system is slowly turning on the insulin.
Here’s what most people get wrong: sweating, shaking, or feeling anxious after an insulin shot? That’s low blood sugar - not an allergy. True allergic reactions involve your immune system, not your blood glucose levels.
What’s Really Causing the Reaction?
You might think it’s the insulin itself. But often, it’s not.Modern insulin is highly purified. The molecule has changed a lot since the 1920s, when animal insulin caused allergies in up to 15% of users. Today, most reactions come from the additives - the stuff that keeps the insulin stable. Two common culprits: metacresol and zinc.
For example, Humalog has more metacresol than other insulins. If you’ve switched to Humalog recently and started getting rashes or swelling, that could be why. Some people react to preservatives, not the insulin. That’s good news - because if you switch to a different brand with different additives, your symptoms might disappear.
And here’s another twist: some people react to the needle or the alcohol swab. A patch test can help rule that out. But if the reaction only happens when you inject insulin, then it’s the insulin or its ingredients.
How Do Doctors Confirm It?
You can’t diagnose this yourself. You need testing.A specialist - usually an allergist - will do one of two things:
- Skin prick test: A tiny drop of insulin is placed on your skin, then lightly pricked. If you’re allergic, a red bump appears within 15-20 minutes.
- Specific IgE blood test: This checks for antibodies that signal an immediate allergic response. It’s less sensitive than skin testing but useful if you’re on antihistamines or have severe skin conditions.
For delayed reactions, there’s no simple test. Doctors look at your history: when did the symptoms start? How long after the injection? Did they happen with every insulin type? They’ll compare your reaction timeline with known patterns.
Don’t wait. If you suspect an allergy, talk to your diabetes team immediately. Stopping insulin on your own can lead to diabetic ketoacidosis - a life-threatening condition.

What Can You Do About It?
There are three main paths forward - and the right one depends on your reaction type.1. Switch Insulin Types
This works in about 70% of cases. If you’re on a human insulin like NPH or regular insulin, try switching to a modern analog - like insulin glargine, detemir, or degludec. These are less likely to trigger reactions. If you’re already on an analog, switch to a different brand. For example, if you’re on Humalog, try NovoRapid or Fiasp. The excipients are different. You might be reacting to metacresol in one but not another.
2. Use Topical Treatments for Delayed Reactions
If you’re getting bruising, hard lumps, or joint pain that shows up hours after your shot, try this: right after injecting, apply a topical calcineurin inhibitor like tacrolimus or pimecrolimus. Do it again 4-6 hours later. These creams calm the immune response in the skin without suppressing your whole body.
For more stubborn cases, your doctor might prescribe a mid-to-high potency steroid cream like flunisolide 0.05%. Apply it the same way - immediately and again later. This can reduce inflammation and prevent long-term tissue damage.
3. Insulin Desensitization
If switching doesn’t work, and you absolutely need insulin, desensitization might be your only option. This is done under medical supervision. You start with a tiny, diluted dose of insulin - sometimes as little as 0.001 units - and slowly increase it over hours or days. Your body learns not to react.
Studies show this works in about two-thirds of cases. One study of four patients found that symptoms disappeared completely in two and improved in the other two. But it’s not easy. You need to be monitored closely for hours. Blood sugar can swing wildly. That’s why it’s usually done in a hospital or clinic with glucose monitoring and emergency meds on hand.
When to Call Emergency Services
If you have any of these symptoms - right after injecting insulin - call emergency services immediately:
- Swelling of your lips, tongue, or throat
- Difficulty breathing or wheezing
- Dizziness or fainting
- Sudden skin discoloration or hives spreading beyond the injection site
This is anaphylaxis. Don’t drive yourself to the hospital. Call 999 (or your local emergency number). Use an epinephrine auto-injector if you have one. Waiting even 10 minutes can be deadly.
What Not to Do
There are a few dangerous myths floating around:
- Don’t stop insulin. Even if you’re reacting, stopping can cause DKA - especially if you have type 1 diabetes. Your body needs insulin to survive.
- Don’t assume it’s just irritation. Repeated localized reactions can lead to lipohypertrophy - fatty lumps under the skin that mess up insulin absorption and make blood sugar harder to control.
- Don’t ignore delayed symptoms. Joint pain or bruising that lasts weeks isn’t normal. It’s your immune system signaling a problem.
What’s New in Insulin Allergy Management?
Things are improving. Newer insulin formulations are being designed with fewer allergenic additives. Some companies are testing versions without metacresol altogether. Continuous glucose monitors (CGMs) are making desensitization safer - doctors can watch your blood sugar in real time as they slowly increase your dose.
Researchers are also looking for biomarkers - blood tests that could predict who’s at risk before they even react. That’s still experimental, but it’s coming.
For now, the key is awareness. If you’ve had any unusual reaction after injecting insulin - even once - talk to your doctor. Don’t wait for it to get worse. You’re not being dramatic. You’re being smart.
Keeping Track Helps
Start a simple log: write down the date, time, insulin brand, dose, and what happened. Did the reaction happen only with one type? Did it happen after a new batch? Did it get worse over time? Bring this to your appointment. Patterns matter.
And remember: you’re not alone. Even though insulin allergies are rare, they’re real. And with the right help, you can keep using insulin safely - no matter what your body throws at you.
Can you develop an insulin allergy after years of using it without problems?
Yes. While most insulin allergies show up early, delayed reactions can occur even after 10 or more years of use. These are often T-cell mediated and may present as joint pain, muscle aches, or persistent bruising at injection sites - not the immediate swelling or hives you’d expect. This is why long-term users shouldn’t dismiss new symptoms as just "aging skin" or "injection trauma."
Is insulin allergy the same as an insulin side effect?
No. Common side effects like sweating, trembling, or hunger are signs of low blood sugar - not an immune reaction. An insulin allergy involves your immune system responding to the insulin or its additives, causing symptoms like hives, swelling, or breathing trouble. Side effects are predictable and tied to dosage. Allergies are unpredictable and can happen even with small doses.
Can you outgrow an insulin allergy?
Not really. Insulin allergies don’t fade on their own. But they can be managed. Many people switch insulin types or use desensitization to tolerate insulin again. Once you’ve had a true allergic reaction, your immune system remembers it. Avoiding insulin entirely isn’t an option for most people with type 1 diabetes - so the goal is to retrain your body’s response, not wait for it to go away.
Are newer insulins less likely to cause allergies?
Yes. Modern analog insulins (like glargine, detemir, degludec) are more purified than older animal or human insulins. They have fewer impurities and are less likely to trigger immune responses. However, they still contain additives like metacresol or zinc, which can cause reactions in sensitive people. Switching between analog brands - not just from human to analog - can help if you’re reacting to a specific preservative.
What if I can’t switch insulin or do desensitization?
For people with type 2 diabetes, oral medications like metformin or GLP-1 agonists may be an option if insulin isn’t essential. But for type 1 diabetes, insulin is life-saving - there’s no alternative. In these cases, desensitization is the standard path forward. If that fails, specialized centers may explore experimental options like monoclonal antibody therapy or ultra-pure insulin formulations not yet widely available. Never stop insulin without medical supervision.
Can I use antihistamines to treat insulin allergies?
For mild, localized reactions - yes. Oral antihistamines like cetirizine or loratadine can reduce itching and swelling. But they won’t stop anaphylaxis. For systemic reactions, you need epinephrine and emergency care. Antihistamines are a band-aid, not a solution. Always follow up with an allergist to find the root cause.
11 Comments
Write a comment
More Articles

Antidepressant Overdose: Recognizing Serotonin Syndrome Warning Signs Before It's Too Late
Serotonin syndrome is a life-threatening reaction to too much serotonin, often caused by antidepressant overdose or drug interactions. Know the warning signs - tremors, clonus, high fever - and act fast.



Sidra Khan
December 22, 2025 AT 15:21I’ve been on Lantus for 8 years and just started getting these weird itchy lumps last month. Thought it was stress or my shirt rubbing. Turns out it’s metacresol. Switched to Basaglar and poof. Gone. Why didn’t my endo mention this?