What Happens When Your Blood Sugar Drops Too Low
You take your diabetes medication as directed, eat on time, and still wake up shaky, sweaty, and confused. Or maybe you feel fine until you suddenly can’t think straight while driving. This isn’t bad luck-it’s hypoglycemia, a dangerous side effect of certain diabetes drugs. Blood glucose below 70 mg/dL triggers warning signs like trembling, hunger, and rapid heartbeat. If it drops below 54 mg/dL, you risk confusion, seizures, or loss of consciousness. And it’s more common than most people realize: up to 40% of people using insulin or sulfonylureas experience at least one episode per year.
Which Diabetes Medications Cause the Most Problems
Not all diabetes drugs carry the same risk. Some are much safer than others. If you’re on insulin-whether it’s long-acting, rapid-acting, or a mix-you’re at the highest risk. Sulfonylureas like glimepiride and glyburide are next, with 15-30% of users having low blood sugar episodes annually. Meglitinides (nateglinide, repaglinide) also spike insulin quickly, making them risky if meals are skipped.
On the flip side, metformin alone rarely causes hypoglycemia (less than 5% risk). GLP-1 receptor agonists (like semaglutide) and SGLT2 inhibitors (like empagliflozin) are even safer, with risks under 3%. If you’re frequently going low, talk to your doctor about switching to a lower-risk option. It’s not about giving up control-it’s about staying safe while still managing your numbers.
Who’s Most at Risk-and Why
Hypoglycemia doesn’t pick favorites, but some people are far more vulnerable. If you’re over 65, your risk jumps by 40%. Kidney problems? Your risk triples. Been living with diabetes for more than 15 years? You’re 50% more likely to have trouble recognizing when your blood sugar drops. That’s called hypoglycemia unawareness-and it affects 25% of type 1 patients and 10% of type 2 patients after long-term disease.
Another hidden danger: beta-blockers. Many people take these for high blood pressure or heart conditions, but they silence the body’s early warning signs-no sweating, no shaking. You won’t feel it coming until it’s too late. Alcohol is another silent killer. One drink can block your liver’s ability to release glucose, leading to a crash hours later, especially overnight.

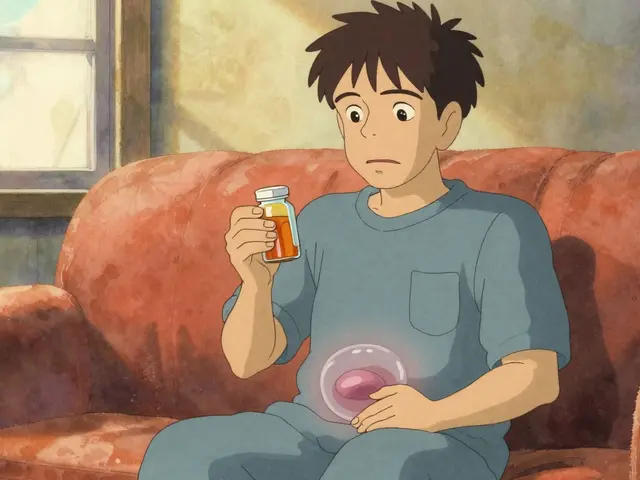
The 15-15 Rule-And Why Most People Get It Wrong
When your blood sugar dips below 70 mg/dL, the standard fix is the 15-15 rule: consume 15 grams of fast-acting carbs, wait 15 minutes, then check again. Simple, right? But here’s the catch: 63% of people use the wrong stuff. They reach for candy bars, juice boxes with added sugar, or worse-artificial sweeteners. None of those work fast enough.
Use glucose tablets (14g per tablet), gel, or regular soda (not diet). Four glucose tablets, 4 oz of juice, or 1 tablespoon of honey will raise your blood sugar quickly. Don’t overdo it. Eating too much can send your sugar sky-high. And never skip the recheck. Many people feel better after 10 minutes and assume they’re fine. But blood sugar can drop again. Wait the full 15 minutes.
Tools That Actually Work-And What They Cost
Technology is changing how people manage low blood sugar. Continuous glucose monitors (CGMs) like Dexcom G7 or Freestyle Libre 3 track your levels every 5 minutes and alert you before you crash. Studies show they cut severe hypoglycemia by nearly half. But they’re expensive: $89 a month for Libre 3, $399 every quarter for Dexcom. Medicare now covers them for insulin users, but out-of-pocket costs still block 35% of low-income patients.
Smart insulin pens (like InPen or NovoPen 6) track doses and sync with apps. Glucagon emergency kits are non-negotiable if you’re on insulin. New nasal spray versions like Baqsimi work in seconds-no mixing, no needles. They cost around $250, but many insurance plans now cover them. Keep one in your bag, car, and workplace. And don’t forget your partner or coworker should know how to use it.
Real-Life Strategies That Prevent Crashes
People who avoid frequent lows don’t just rely on meds-they build habits. The most successful users do three things:
- Keep a hypo bag everywhere: car, desk, purse, gym bag. Inside: glucose tablets, a note with emergency contacts, and glucagon.
- Set phone alarms for meals and snacks-even if you’re not hungry. Skipping meals causes 42% of hypoglycemia episodes reported on diabetes forums.
- Log every low event. Not just the number, but what you ate, when you took meds, how much you moved. People who log consistently reduce episodes by 37% in three months.
One man in Sydney, 72, with type 2 diabetes and kidney issues, started using a simple notebook after three nighttime crashes. He wrote down: “Glyburide 5mg at 8am, ate toast at 8:30, walked 20 mins at 10am, BG dropped to 58 at 11:15.” His doctor adjusted his dose and switched him to glimepiride. Within two months, no more lows.

When to Call for Help-and When to Act Alone
Level 1 hypoglycemia (below 70 mg/dL) can usually be fixed by you. Level 2 (below 54 mg/dL) needs immediate action, even if you feel fine. Level 3 means you’re unconscious, confused, or seizing. That’s an emergency. No one should try to treat you with food or drink if you can’t swallow. That’s when glucagon kicks in.
Teach your family, coworkers, or roommates how to use your glucagon kit. Practice with a trainer pen. If you live alone, consider a medical alert system. In Australia, some Medicare-funded programs offer subsidized alarms for high-risk patients.
What Your Doctor Should Be Asking You
Too often, doctors focus only on HbA1c numbers. But that’s not enough. A reading of 7% might look good-but if you’re crashing to 40 mg/dL twice a week, that’s dangerous. The American Diabetes Association now recommends asking four key questions at every visit:
- Have you had any episodes of low blood sugar in the past month?
- Did you need help from someone else to treat it?
- Did it happen during sleep, exercise, or after skipping a meal?
- Are you using a CGM or checking your blood sugar regularly?
They should also use the 8-point hypoglycemia risk score. It’s quick, proven, and predicts severe events with 82% accuracy. If you’re over 65, have kidney issues, or take multiple meds, your target blood sugar should be higher-80-130 mg/dL-not the old 70-130 standard.
What’s Coming Next
The future of hypoglycemia management is smarter, faster, and more automatic. New systems like Tandem’s Control-IQ pump adjust insulin automatically based on CGM data, cutting nighttime lows by over 3 hours. AI-driven dosing algorithms are being tested and could reduce hypoglycemia by 60% in the next few years. And dasiglucagon, a new liquid glucagon that doesn’t need mixing, just hit a button-it’s already FDA-approved and changing emergency care.
But none of this matters if you don’t know your risks, don’t carry treatment, or don’t talk to your doctor. Hypoglycemia isn’t a glitch-it’s a signal. Listen to it. Adjust. Protect yourself. Your life depends on it.
14 Comments
Write a comment
More Articles

Opioid Reactions: How to Tell Itching from a True Allergy and What to Do
Most opioid itching isn't an allergy - it's a side effect. Learn how to tell the difference, which opioids cause less itching, and what to do if you're labeled allergic when you're not.
Crohn's Disease and Gluten Intolerance: Key Signs and What to Watch For
Explore the link between Crohn's disease and gluten intolerance, learn warning signs, testing methods, and dietary steps to manage symptoms effectively.
Anticholinergics and Urinary Retention: How Prostate Issues Make Medication Risks Worse
Anticholinergics for bladder issues can worsen urinary retention in men with prostate enlargement. Learn how these medications interact with BPH, the risks involved, and safer alternatives. Includes real-world data, expert advice, and management strategies.

Brad Seymour
November 8, 2025 AT 09:37This is actually one of the clearest breakdowns I’ve seen on hypoglycemia. I’ve been on glimepiride for 8 years and had two scary episodes last winter. Switching to metformin + GLP-1 was a game changer. No more 3 a.m. panic attacks.
Also, the 15-15 rule? So many people think candy bars work. Nope. Glucose tabs are the only real fix.