Opioid-Induced Adrenal Insufficiency Risk Calculator
Why This Matters
Long-term opioids (>20 MME/day for >90 days) can suppress your body's stress response. Symptoms like fatigue and dizziness are often missed as early signs of adrenal insufficiency - a life-threatening condition.
Your Risk Level
Risk Factors
Symptoms
- Chronic fatigue
- Nausea and loss of appetite
- Dizziness when standing
- Muscle weakness
- Low mood
High Risk? Consult your physician immediately about adrenal function testing. Untreated OIAI can lead to fatal adrenal crisis.
Most people know opioids can cause constipation, drowsiness, or dependence. But few know that long-term opioid use can quietly shut down your body’s natural stress response - leading to a condition called opioid-induced adrenal insufficiency (OIAI). It’s rare. It’s subtle. And if missed, it can kill you.
What Exactly Is Opioid-Induced Adrenal Insufficiency?
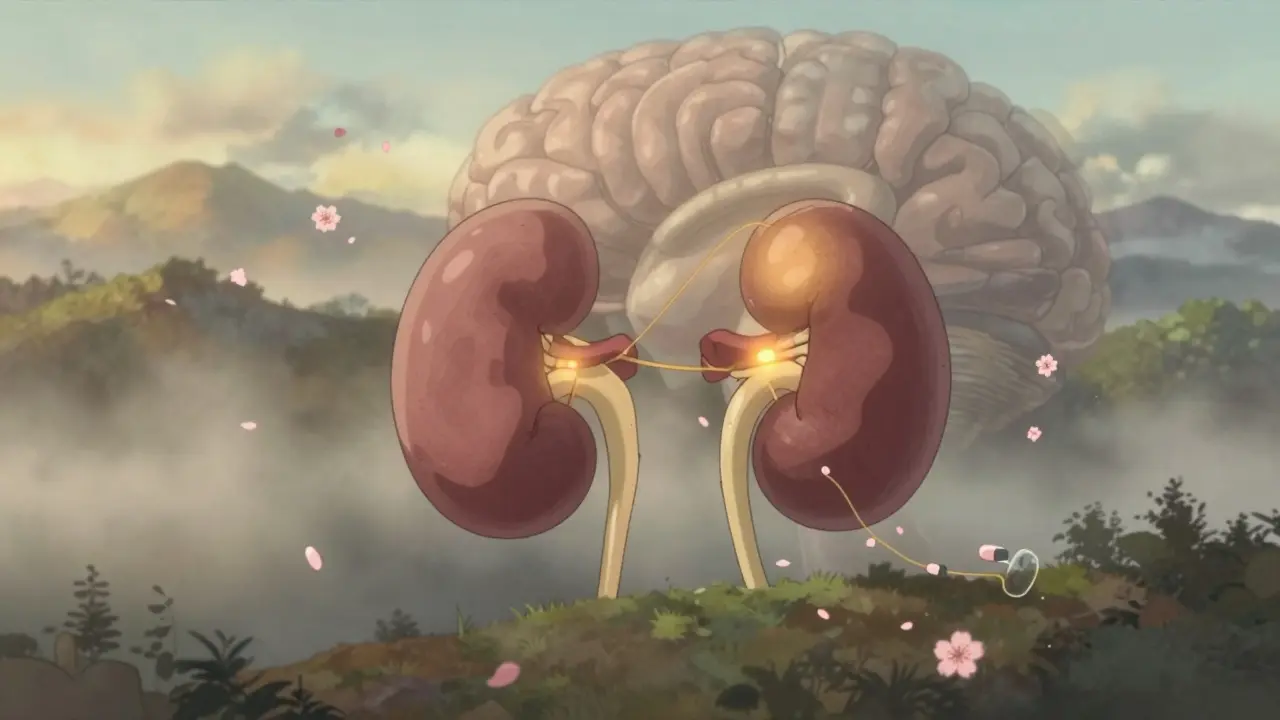
Your adrenal glands sit on top of your kidneys and produce cortisol - the hormone that keeps you alive during stress. Whether you’re in a car accident, fighting an infection, or having surgery, cortisol kicks in to raise your blood pressure, stabilize your blood sugar, and calm inflammation. Without it, your body can’t respond. That’s adrenal insufficiency. Opioids don’t damage your adrenals. Instead, they silence the chain of command: the hypothalamus and pituitary gland. These brain regions normally signal the adrenals to make cortisol. But opioids bind to receptors in the brain and block that signal. No signal = no cortisol. It’s like cutting the wire to a smoke alarm - the alarm still works, but no one’s telling it to go off. This isn’t new science. Studies from the 2010s already showed opioids suppress ACTH and cortisol. But for years, doctors didn’t connect the dots. Patients showed up tired, nauseous, low-blood-pressure, and were told they were just depressed or had the flu. Turns out, their bodies had run out of stress fuel.Who’s at Risk?
You don’t need to be on heroin. Prescription opioids are the main culprit. About 5% of adults in the U.S. are on chronic opioid therapy - that’s over 16 million people. And while not everyone develops adrenal insufficiency, the risk climbs sharply with dose and duration. If you’re taking more than 20 morphine milligram equivalents (MME) per day for longer than 90 days, your risk goes up. One study of 162 chronic opioid users found 5% had OIAI. Another, looking at patients on methadone or high-dose oxycodone, found 22.5% failed adrenal stimulation tests - compared to 0% in healthy controls. It doesn’t matter if you’re on oxycodone, hydrocodone, morphine, or methadone. All of them can do this. Even fentanyl patches. The key factors? Dose. Duration. And whether your body’s been under constant chemical suppression.What Are the Symptoms? (And Why They’re Easy to Miss)
OIAI doesn’t come with a flashing red light. Its symptoms look exactly like other things:- Chronic fatigue - "I’m just tired all the time"
- Nausea, loss of appetite - "I guess my pain is making me eat less"
- Dizziness when standing - "Must be low blood pressure from meds"
- Muscle weakness - "I’m getting older"
- Low mood - "I’m depressed from chronic pain"

How Is It Diagnosed?
There’s no blood test you can take at your GP’s office and get an instant answer. Diagnosis requires a stimulation test. The gold standard is the ACTH stimulation test. You get a shot of synthetic ACTH. Then, your cortisol levels are checked at 30 and 60 minutes. If your cortisol stays below 18 mcg/dL (or 500 nmol/L), your adrenals didn’t respond - meaning your brain isn’t telling them to work. Some newer research suggests even lower thresholds might be more accurate. A morning cortisol under 3 mcg/dL is a strong red flag, especially if you’re on high-dose opioids. The problem? Most doctors don’t order this test. Not unless they’re endocrinologists. And most pain clinics don’t screen for it. That’s why so many cases go undetected until it’s too late.Can It Be Reversed?
Yes. And that’s the good news. In one case, a 25-year-old man developed severe hypercalcemia after a critical illness. His doctors couldn’t figure out why - until they checked his cortisol. It was undetectable. He’d been on methadone for chronic pain. Once they stopped the methadone and gave him hydrocortisone, his cortisol returned to normal within weeks. His calcium levels stabilized. He recovered fully. This isn’t an outlier. Multiple case reports show the same pattern: stop or taper the opioid, give glucocorticoids during the transition, and the HPA axis slowly wakes up. It can take weeks to months. But the glands aren’t broken. They’re just asleep. Important note: you can’t just quit opioids cold turkey if you have OIAI. Your body needs steroid cover during withdrawal. Otherwise, you risk adrenal crisis. That’s why this needs to be managed by a doctor - not self-managed.What About Aldosterone? Do Opioids Affect Salt Balance?
Good question. Aldosterone is another hormone made by the adrenals. It controls sodium and potassium. Low aldosterone causes salt wasting, low blood pressure, and high potassium. Here’s the relief: opioids don’t suppress aldosterone. That’s because aldosterone is controlled by a different system - the renin-angiotensin system - not the HPA axis. So if you have low cortisol but normal sodium and potassium, that’s consistent with OIAI. If your potassium is high and sodium is low? Something else is going on.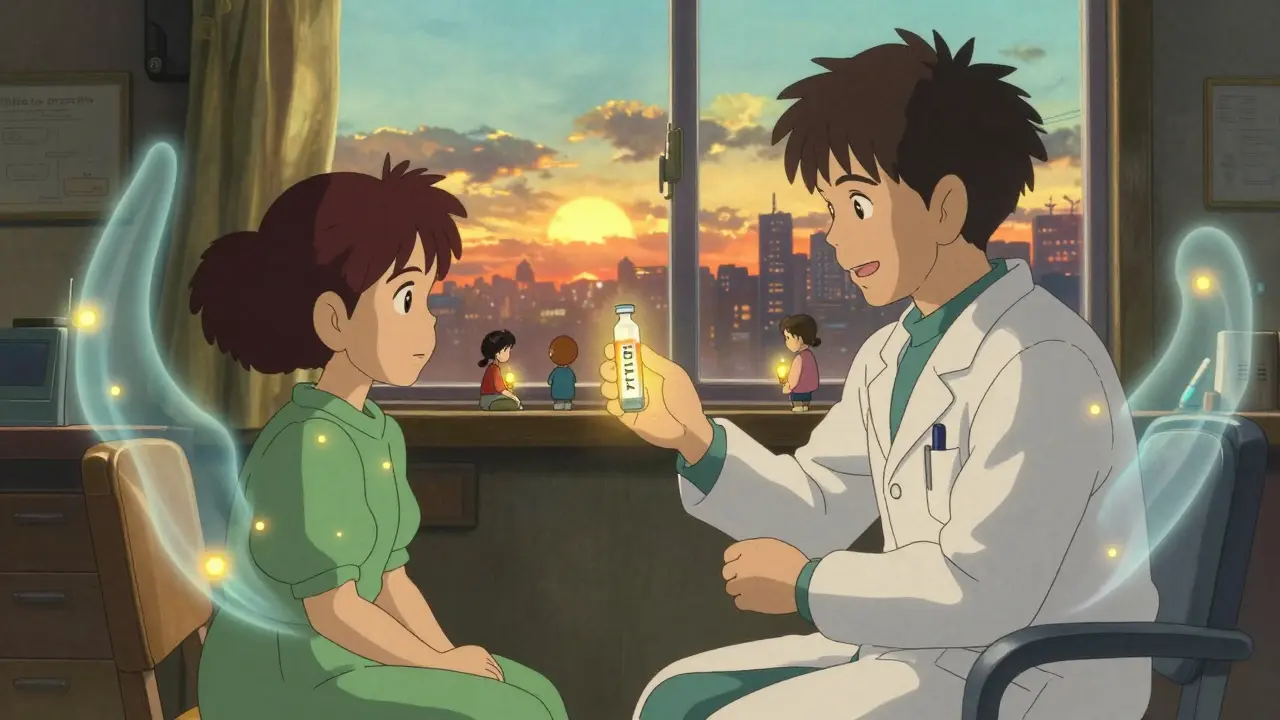
Why Isn’t This More Widely Known?
Because it’s invisible until it’s deadly. The opioid epidemic has focused on overdoses, addiction, and withdrawal. But the slow, silent damage - like hormonal shutdown, low testosterone, and adrenal insufficiency - gets ignored. Studies show patients on long-term opioids report worse quality of life across physical, emotional, and social domains. Some of that is pain. Some of it is cortisol deficiency. Clinicians aren’t taught this in medical school. Guidelines don’t recommend routine screening. And when a patient says, "I’m always tired," the default answer is "depression" or "sleep apnea." Not "your adrenals stopped working because of your pain meds." But awareness is growing. Papers from 2020 to 2024 are calling for better screening. The American Medical Association’s Ed Hub now explicitly says: "Concern for OIAI should be raised in patients on chronic opioid therapy, particularly over 20 MME daily, with signs of adrenal insufficiency."What Should You Do If You’re on Long-Term Opioids?
If you’ve been on opioids for more than three months - especially at doses above 20 MME daily - and you feel constantly tired, dizzy, nauseous, or weak, ask your doctor one simple question: "Could this be opioid-induced adrenal insufficiency? Can we check my cortisol?" Don’t wait for a crisis. Don’t assume it’s "just pain." This is a treatable condition. And if caught early, it’s completely reversible. If your doctor doesn’t know what you’re talking about, bring them the research. Print out the 2024 review from Frontiers in Endocrinology. Point them to the ACTH stimulation test. Most will agree to order it if you’re persistent. And if you’re a clinician reading this? The next time someone on long-term opioids says they’re exhausted - don’t reach for the antidepressant. Reach for the cortisol test.Final Thought: It’s Not About Stopping Opioids - It’s About Safe Use
This isn’t a call to stop opioids. For many, they’re the only thing keeping pain manageable. But they’re not harmless. Every medication has trade-offs. Opioids help with pain. But they can also shut down your body’s emergency system. The goal isn’t fear. It’s awareness. If you’re on opioids long-term, your care team should be watching your hormones - not just your pain score. Because you can’t survive a crisis if your body has forgotten how to respond to one.11 Comments
Write a comment
More Articles

The Role of Psychological Counseling in Dementia of the Alzheimer's Type Care
In my latest blog post, I discuss the vital role psychological counseling plays in the care of individuals with Alzheimer's-type dementia. I highlight how counseling not only supports patients in coping with the emotional and cognitive challenges of the disease but also provides essential guidance to their caregivers. Furthermore, I emphasize the importance of early intervention to maximize the benefits of counseling. Through my research, I've discovered that psychological counseling can significantly improve the overall quality of life for both patients and their families. So, let's spread awareness about the invaluable support that counseling can offer in Alzheimer's care.


Branden Temew
January 1, 2026 AT 21:42So let me get this straight - we’ve got a whole class of drugs that can turn your body’s emergency button into a mute switch, and the medical system’s still acting like it’s just a bad Yelp review? 😅
It’s like giving someone a chainsaw and then being shocked when they forget how to use a hammer.