
When cancer pain won’t go away, what actually helps?
Imagine waking up every morning with aching bones, nausea that won’t leave, and the fear that no one understands how bad it feels. This isn’t rare. About 70-90% of people with advanced cancer experience pain that’s not properly managed. Too often, it’s dismissed as "just part of the disease." But it doesn’t have to be this way. The truth is, 80-90% of cancer pain can be controlled with the right approach - not just with pills, but with a full plan that puts the person back in charge of their life.
Why pain gets ignored - and why that’s dangerous
Doctors don’t ignore pain on purpose. But the system is built in a way that makes it easy to miss. Many oncologists focus on shrinking tumors, not easing suffering. Patients, especially older adults or those from cultures that value stoicism, often stay quiet because they don’t want to be a burden. A 2017 study found that 40% of oncology nurses hadn’t been trained in current pain management practices. And patients? 65% fear addiction more than the pain itself.
This silence costs lives. Untreated pain doesn’t just make days miserable - it weakens the immune system, blocks sleep, and makes it harder to eat or move. It pulls people away from family, from joy, from even the smallest pleasures. Pain that’s not addressed isn’t just physical. It’s emotional, social, and spiritual.
The three-step ladder that changed everything
In 1986, the World Health Organization laid out a simple idea that became the foundation of modern cancer pain care: the three-step analgesic ladder. It’s still used today because it works.
- Step 1 (Mild pain): Start with acetaminophen (up to 4,000 mg/day) or ibuprofen (400-800 mg three times a day). These are safe for most people and help with inflammation and dull, constant pain.
- Step 2 (Moderate pain): Add a weak opioid like codeine (30-60 mg every 4 hours) if the first step isn’t enough. This isn’t a big jump - it’s a bridge.
- Step 3 (Severe pain): Use strong opioids like morphine (5-15 mg every 4 hours orally). This isn’t a last resort - it’s the right step when pain is this bad.
Key point: Opioids aren’t scary if used correctly. The goal isn’t to make someone numb - it’s to let them sleep, talk to their kids, eat a meal, or sit outside. Doses are adjusted every 24-48 hours until pain drops below a 4 on a 0-10 scale. Breakthrough pain? A quick dose of 10-15% of your daily total is all it takes.
It’s not just pills - the other tools that work
Pain isn’t just about nerves firing. Sometimes, it’s because a tumor is pressing on a bone, a nerve, or a spinal cord. That’s where non-drug treatments come in.
- Radiotherapy: A single 8 Gy radiation dose to a bone metastasis can cut pain by half in days. It’s fast, targeted, and often covered by insurance.
- Bisphosphonates: Drugs like zoledronic acid (given IV every 3-4 weeks) help strengthen bones weakened by cancer and reduce fracture risk.
- Anticonvulsants: Gabapentin (100-1,200 mg three times daily) works wonders for nerve pain - the burning, shooting kind that opioids don’t touch.
- Antidepressants: Duloxetine (30-60 mg daily) helps with both nerve pain and the low mood that often comes with chronic illness.
- Corticosteroids: Dexamethasone (4-16 mg daily) reduces swelling around tumors, easing pressure and pain.
And don’t forget the basics: heat packs, gentle massage, music therapy, and even guided breathing can lower pain scores by 20-30%. These aren’t "nice-to-haves." They’re part of the treatment plan.
When opioids don’t work - or cause new problems
Not everyone responds the same way. Some people get nauseous. Others feel foggy. A few develop something called opioid-induced hyperalgesia - where the pain actually gets worse because of the medication. This happens in 15-20% of long-term users.
When that happens, you don’t stop treatment. You switch. Doctors use equianalgesic tables to convert from morphine to fentanyl or methadone, starting at 50-75% of the calculated dose because the body hasn’t fully adjusted. This isn’t failure - it’s smart adaptation.
And yes, there’s a risk of overdose. But the CDC’s guidelines now make a clear exception for cancer: the rules for chronic non-cancer pain don’t apply here. If you have cancer, your priority is comfort - not avoiding opioids at all costs.
Quality of life isn’t a buzzword - it’s the goal
One study showed that when patients got help from a palliative care team within 8 weeks of diagnosis, their quality of life improved by 20-30%. They were less depressed, slept better, and even lived longer - by an average of 2.5 months.
Why? Because palliative care doesn’t just treat pain. It asks: What matters to you?
Is it being able to walk to the garden? Watching your grandchild’s soccer game? Having a conversation without crying? These aren’t small things. They’re everything. Palliative teams include social workers, chaplains, and psychologists who help patients and families talk about fears, goals, and what comes next.
And it’s not just for the last weeks of life. The best time to start palliative care? Now. Not when everything falls apart. Not when the pain is unbearable. Now.
What gets in the way - and how to push past it
Even with all the science, real-world barriers still block care:
- Provider knowledge gaps: Too many clinicians still think opioids are risky. Training helps. Hospitals that require 8 hours of annual palliative care training see 35% better pain control.
- Cultural silence: In some Asian and Hispanic communities, 28% of patients hide their pain because they believe suffering is noble. Families need education - not judgment.
- Insurance limits: Many plans won’t cover acupuncture, massage, or counseling. Ask for exceptions. Fight for it. Your comfort is medical, not optional.
- Regulatory confusion: Some pharmacies refuse to fill opioid prescriptions because they’re afraid of audits. Bring your doctor’s note. Know your rights.
There’s a new tool making a difference: smartphone apps that let patients log pain levels, side effects, and mood in real time. A 2021 study found these apps improved documentation accuracy by 22%. That means doctors see the full picture - not just what’s remembered at the next appointment.
What’s next? Science is moving fast
Researchers are testing new drugs that target cancer pain at the source - not just the nerves, but the bone destruction and inflammation caused by tumors. Twelve new agents are in Phase II or III trials as of late 2023.
Genetic testing is starting to help too. Some people metabolize opioids slowly because of their CYP450 genes. Testing can tell doctors, "Start with half the dose." That’s precision medicine - and it’s already here.
Artificial intelligence is being trained to predict pain spikes before they happen. Imagine a system that says, "Based on your sleep, activity, and recent scans, you’re likely to have increased pain tomorrow. Here’s a plan." That’s not science fiction. It’s coming.
What you can do today
You don’t need to wait for permission to ask for help.
- Ask your oncologist: "Have you screened me for pain today?" (It’s required by NCCN guidelines.)
- Use the 0-10 scale. Don’t say "it hurts." Say "it’s a 7."
- Request a palliative care consult. You don’t need to be dying to get it.
- Track your pain for a week. Note when it’s worse, what helps, what makes it worse.
- Bring a family member to appointments. They’ll remember things you miss.
Pain doesn’t have to be your constant companion. You deserve to breathe without gritting your teeth. To laugh without fear. To hold someone’s hand without flinching. That’s not a luxury. It’s care.
Is palliative care the same as hospice?
No. Hospice is for people in the final months of life who are no longer receiving curative treatment. Palliative care is for anyone with a serious illness - even if they’re still getting chemotherapy, surgery, or radiation. You can start palliative care the day you’re diagnosed. It’s about living better, not just dying peacefully.
Will opioids make me addicted?
For people with cancer, the risk of addiction is very low - less than 1%. What you’re managing is physical dependence, not addiction. Addiction is compulsive drug use despite harm. Cancer patients take opioids to relieve pain, not to get high. Doctors monitor for side effects, not just for addiction. If your pain is controlled and you’re not using more than prescribed, you’re not addicted.
What if my doctor won’t prescribe enough pain medicine?
You have the right to effective pain control. Ask for a referral to a palliative care specialist or pain management clinic. If your doctor refuses, get a second opinion. Many hospitals have palliative care teams that can step in directly. Don’t let fear or outdated beliefs stop you from feeling better.
Can non-drug methods really help with cancer pain?
Yes. Studies show that techniques like acupuncture, massage, meditation, and music therapy can reduce pain scores by 20-40%. They work best when used with medication, not instead of it. They help your body relax, reduce stress hormones, and improve sleep - all of which make pain easier to handle.
How do I know if my pain plan is working?
Ask yourself: Can I sleep through the night? Can I eat without nausea? Can I talk to my family without crying? If the answer is no, your plan needs adjusting. Pain is considered controlled when it’s at or below a 4 on a 0-10 scale for most of the day. If you’re still at a 7 or higher, talk to your team. There’s always another option.
Are there new treatments on the horizon?
Yes. Researchers are testing drugs that block specific pain signals caused by tumors - like those that attack bone destruction or nerve compression. There are also AI tools that predict pain spikes before they happen, and genetic tests that tell doctors which pain meds will work best for your body. These aren’t far off - some are already being used in clinical trials.
13 Comments
Write a comment
More Articles
Cushing’s Syndrome: Understanding Excess Cortisol and the Role of Surgical Treatment
Cushing’s syndrome is caused by too much cortisol and can lead to serious health problems. Surgery is the most effective cure for tumor-related cases, with high success rates when performed at specialized centers.
Malignant Hyperthermia and Anesthesia: What You Need to Know About This Life-Threatening Reaction
Malignant hyperthermia is a rare but deadly reaction to common anesthesia drugs. Learn the warning signs, how it's treated with dantrolene, why speed saves lives, and what you should ask before surgery.
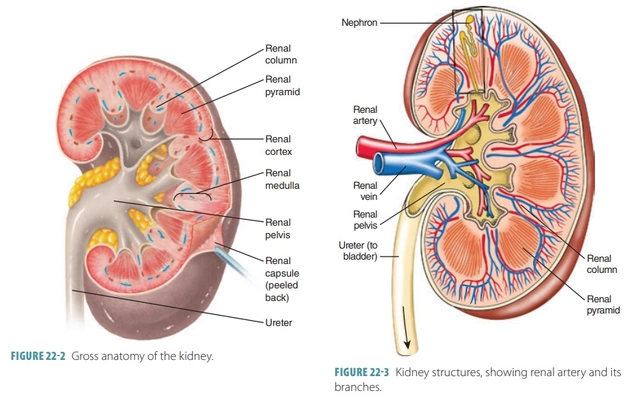
Azathioprine and Kidney Function: What You Should Know
As someone who's always keen on learning about health and medications, I recently came across some vital information on Azathioprine and its impact on kidney function. Azathioprine is an immunosuppressive drug, mainly used to prevent organ rejection after transplantation and to treat autoimmune diseases. While it can be effective for these conditions, it's important to be aware that long-term use may lead to kidney damage, especially in high doses. Regular monitoring of kidney function is essential for those on this medication to ensure they remain healthy. It's always best to discuss any concerns with your healthcare provider to make informed decisions about your treatment options.

steve rumsford
January 7, 2026 AT 12:42this is the kind of post i wish i saw when my dad was going through chemo. why the hell do we still act like pain is something you just gotta suck up?
so many people die in silence because they think being brave means not asking for help. it’s not brave. it’s tragic.