Uveitis Treatment: What Works, What to Avoid, and How to Manage It
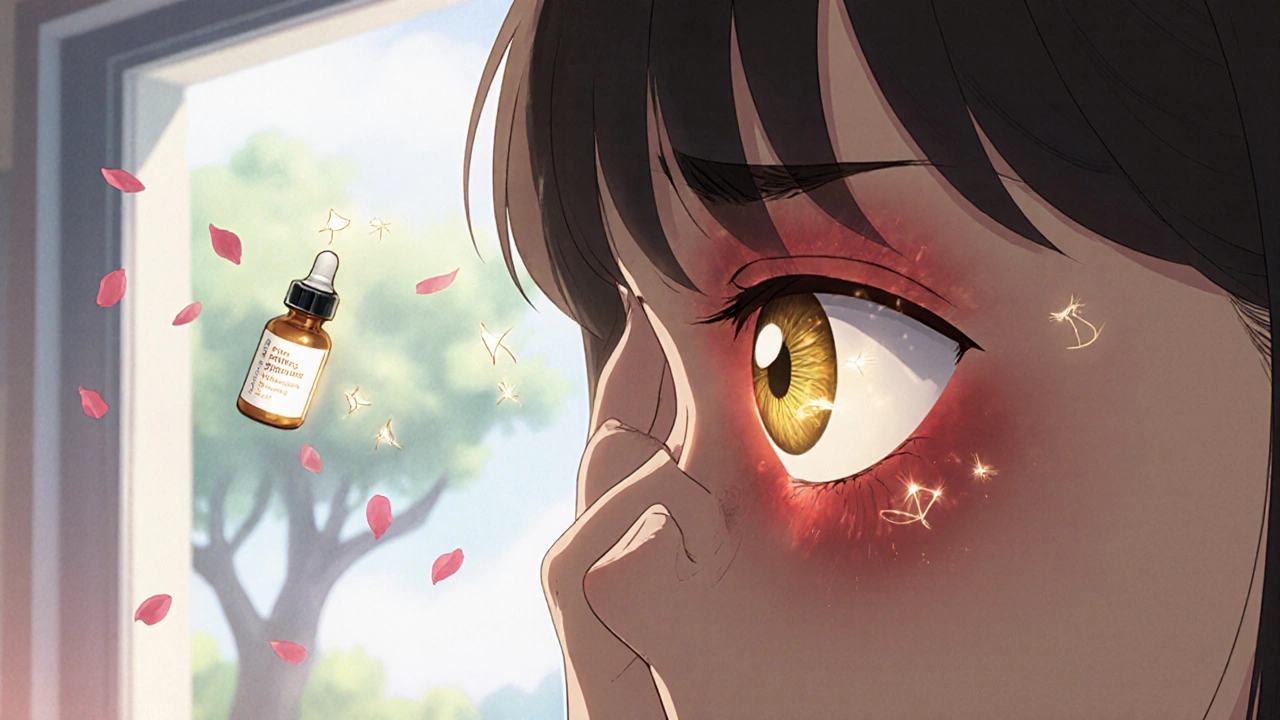
When your eye becomes red, painful, and sensitive to light, it might be uveitis, inflammation of the uvea, the middle layer of the eye that includes the iris, ciliary body, and choroid. Also known as intermediate or posterior uveitis, depending on where the swelling happens, this condition can threaten vision if left untreated. It’s not just a simple eye infection—it’s often tied to autoimmune problems, infections like Lyme disease or herpes, or even conditions like rheumatoid arthritis or sarcoidosis.
Most uveitis treatment, a targeted approach to reduce inflammation and prevent damage to the retina and optic nerve starts with corticosteroids, powerful anti-inflammatory drugs that can be given as eye drops, pills, or injections. But steroids aren’t the whole story. If the inflammation keeps coming back, doctors often turn to immunosuppressants, medications that calm down the overactive immune system—like methotrexate or mycophenolate—to avoid long-term steroid side effects like cataracts or glaucoma. Some newer biologics, originally developed for rheumatoid arthritis, are now being used off-label for stubborn cases, especially when traditional drugs fail.
What you avoid matters just as much as what you take. Skipping follow-ups can let uveitis silently damage your retina. Not treating an underlying infection—like toxoplasmosis or syphilis—means the inflammation will keep flaring. And while over-the-counter painkillers might ease discomfort, they won’t touch the real problem. Uveitis treatment isn’t about quick fixes; it’s about matching the right drug to the root cause, monitoring closely, and staying ahead of complications.
Some people get uveitis after an injury or surgery. Others develop it with no clear trigger. That’s why diagnosis often requires more than just an eye exam—blood tests, imaging, and sometimes even an analysis of eye fluid are needed. The good news? With the right plan, most people keep their vision. The key is catching it early and sticking with the treatment, even when symptoms fade.
In the posts below, you’ll find real-world advice on managing uveitis treatment, from how steroids affect your body long-term to what alternative therapies show promise—and which ones to skip. You’ll also see how other conditions like Crohn’s disease or gout can trigger eye inflammation, and how to avoid dangerous drug interactions when you’re on multiple medications. This isn’t guesswork—it’s what works for real patients, backed by clinical evidence and practical experience.
Uveitis: Understanding Eye Inflammation and Steroid Treatment
Uveitis is a serious eye inflammation that can lead to vision loss if untreated. Learn the signs, causes, and why steroid therapy is the critical first step to saving your sight.