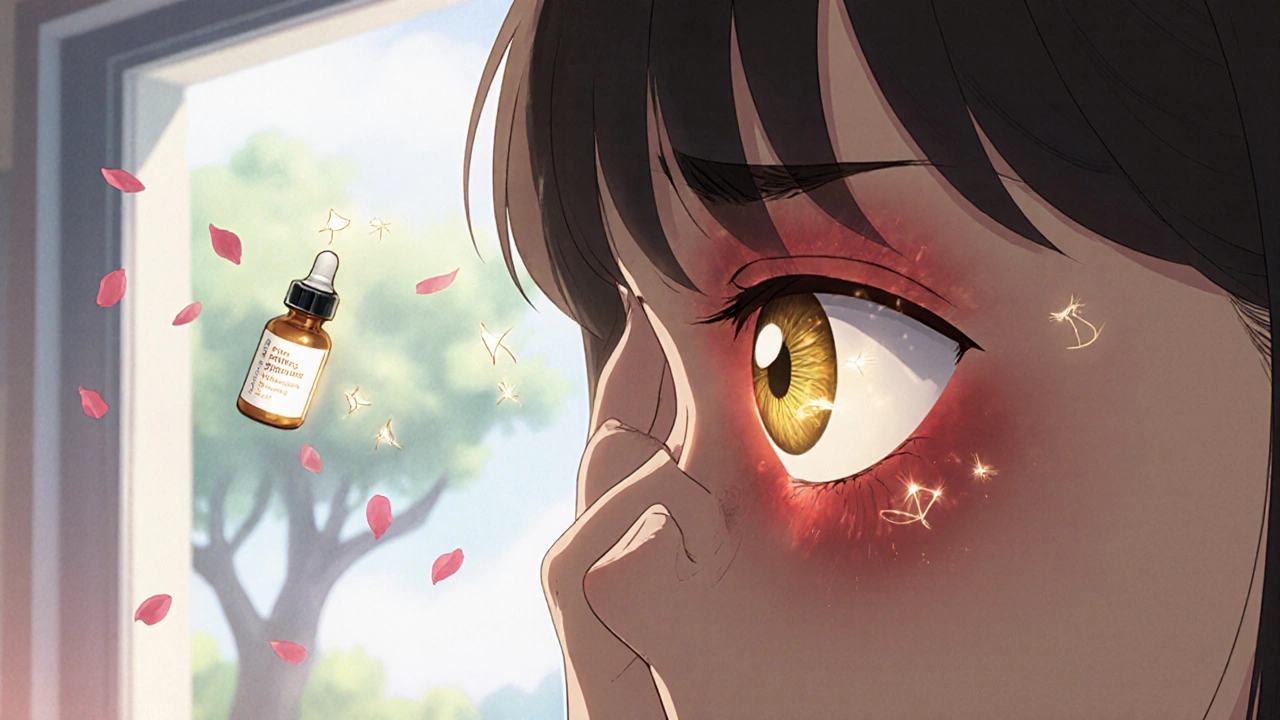
Uveitis isn’t something you can ignore. If your eye suddenly turns red, hurts when you read, or you start seeing floaters like dark spiders crawling across your vision, this could be uveitis - a serious inflammation inside the eye that can steal your sight if left untreated. It’s not just a minor irritation. Uveitis is the third leading cause of blindness worldwide, and for many, it comes without warning. The good news? With fast, correct treatment, especially steroid therapy, most people keep their vision. The key is knowing what to look for - and acting right away.
What Exactly Is Uveitis?
The uvea is the middle layer of your eye. It’s made up of three parts: the iris (the colored part), the ciliary body (which helps focus your lens), and the choroid (a layer full of blood vessels that feeds the retina). When any of these parts get inflamed, that’s uveitis. It’s not one disease - it’s a group of conditions with different causes, locations, and risks. There are four main types, based on where the inflammation happens:- Anterior uveitis - affects the front of the eye (iris and ciliary body). This is the most common type, making up 75% to 90% of cases. It often comes on fast, with pain, redness, and light sensitivity.
- Intermediate uveitis - targets the vitreous, the jelly-like fluid in the middle of the eye. Symptoms are usually floaters and blurry vision, with little to no pain. It can last for years and come back.
- Posterior uveitis - hits the back of the eye, including the retina and choroid. This form is sneaky. It often develops slowly, affects both eyes, and can cause permanent damage before you even notice.
- Panuveitis - inflammation in all layers at once. This is the most severe form and carries the highest risk of vision loss.
What Does Uveitis Feel Like?
Symptoms vary by type, but here’s what to watch for:- Red eye - especially in anterior uveitis. It’s not just a little pink; it’s deep, angry red.
- Pain - often sharp or aching. Many people say it gets worse when reading or focusing up close.
- Light sensitivity - even normal daylight feels blinding. You might squint or want to wear sunglasses indoors.
- Blurred vision - like looking through a foggy window. It doesn’t clear up with glasses.
- Floaters - dark spots, strings, or squiggles drifting across your vision. They’re not just aging; they’re a red flag.
- Loss of vision - especially in posterior uveitis. This isn’t temporary blurriness. It’s a drop in sharpness that doesn’t bounce back.
What Causes Uveitis?
Here’s the hard part: in about half of all cases, doctors can’t find a cause. That’s called idiopathic uveitis. But when they do find one, it usually falls into three buckets:- Autoimmune diseases - your immune system attacks your own eye tissue. Conditions like ankylosing spondylitis, multiple sclerosis, sarcoidosis, and rheumatoid arthritis are common culprits.
- Infections - viruses, bacteria, or fungi trigger inflammation. Herpes simplex, shingles (herpes zoster), syphilis, toxoplasmosis, and cytomegalovirus (CMV) are known triggers.
- Eye injury or surgery - trauma or even a routine cataract operation can spark inflammation in susceptible people.

Steroid Therapy: The First Line of Defense
Steroid therapy is the foundation of uveitis treatment. Steroids - like prednisolone - are powerful anti-inflammatory drugs. They don’t cure the cause, but they calm the fire inside your eye fast. The goal? Stop the inflammation before it scars your eye. How you get the steroids depends on where the inflammation is:- Anterior uveitis - steroid eye drops are the go-to. Drops like prednisolone acetate 1% are used every hour at first, then slowly tapered over weeks. You’ll need close monitoring - too little, and the inflammation returns. Too much, and you risk side effects.
- Intermediate uveitis - eye drops don’t reach deep enough. Doctors often use steroid injections around the eye (periocular) or implants that slowly release medicine inside the eye (intravitreal). Oral steroids may be added if it’s severe or recurring.
- Posterior uveitis and panuveitis - these need systemic treatment. Oral steroids (like prednisone) are common. In some cases, steroid implants are placed directly into the eye. For chronic cases, doctors may add steroid-sparing drugs like methotrexate or mycophenolate to reduce long-term steroid use.
The Hidden Risk: Steroid Side Effects
Steroids save vision - but they can also threaten it. Long-term use carries real risks:- Cataracts - clouding of the eye’s natural lens. Up to 40% of people on long-term steroids develop them.
- Steroid-induced glaucoma - increased eye pressure that damages the optic nerve. This can happen without symptoms until vision is already gone.
- Systemic effects - if you’re taking oral steroids, you might gain weight, get mood swings, or have trouble sleeping. Blood sugar can rise, especially in people with diabetes.
When to See a Doctor - Right Now
Don’t wait for symptoms to get worse. Don’t try to “sleep it off.” Uveitis is a medical emergency. If you have:- Sudden redness in one or both eyes
- Pain that gets worse when reading
- Blurred vision that doesn’t improve
- Floaters that appear out of nowhere
- Extreme sensitivity to light

What Happens If It’s Not Treated?
Untreated uveitis doesn’t just go away. It gets worse. In anterior uveitis, scar tissue forms between the iris and lens. Pupils become misshapen. Fluid can’t drain. Pressure builds. Glaucoma sets in. In posterior uveitis, the retina swells, then scars. Blood vessels leak. The macula - the part of your eye that lets you read faces and recognize colors - gets destroyed. Vision loss here is often permanent. Chronic uveitis, especially intermediate and posterior forms, can lead to retinal detachment, optic nerve damage, and total vision loss. The Lions Eye Institute calls it “a potentially sight-threatening problem” - and they’re right. This isn’t a condition you can hope out of.Living With Uveitis
If you’ve been diagnosed, you’re not alone. Many people manage uveitis for years. But it requires discipline.- Stick to your drop schedule - even if your eye looks fine.
- Attend every follow-up. Pressure checks and scans are non-negotiable.
- Report new symptoms fast - even if they seem minor.
- Protect your eyes from UV light. Wear sunglasses with 100% UV protection.
- Manage stress. While stress doesn’t cause uveitis, it can trigger flares in people with autoimmune triggers.
What’s Next?
If you’ve had uveitis once, you’re at higher risk for another episode. That’s why regular eye exams - even when you feel fine - are critical. If you have an autoimmune disease, work with your rheumatologist and eye doctor together. Communication saves sight. New treatments are coming. More targeted steroid implants. Biologic drugs that block specific immune signals. But right now, the best tool is still early diagnosis and proper steroid use. Don’t gamble with your vision. If something feels off in your eye - get it checked. Today.Can uveitis go away on its own?
No. While symptoms might seem to improve temporarily, the inflammation doesn’t vanish without treatment. Left untreated, it can cause permanent damage to the retina, lens, or optic nerve. Even if your eye looks better, the risk of scarring and glaucoma remains. Always follow through with your doctor’s treatment plan.
Are steroid eye drops safe for long-term use?
Not without monitoring. Long-term use increases the risk of cataracts and steroid-induced glaucoma. That’s why doctors taper the dose slowly and check eye pressure regularly. For chronic cases, steroid-sparing drugs are added to reduce dependency. Never stop or change your drops without consulting your ophthalmologist.
Can uveitis affect both eyes?
Yes. While anterior uveitis often starts in one eye, posterior uveitis and panuveitis usually affect both. Even if only one eye is symptomatic, doctors will examine both because inflammation can develop in the other eye later. If you’ve had uveitis in one eye, you’re at higher risk for it in the other.
Is uveitis the same as pink eye?
No. Pink eye (conjunctivitis) affects the outer surface of the eye and is usually caused by viruses or allergies. It causes redness and discharge but rarely pain or vision changes. Uveitis affects the inner layers, causes deep pain, light sensitivity, and blurred vision. The treatments are completely different. Mistaking uveitis for pink eye can delay critical care.
Can stress cause uveitis?
Stress doesn’t cause uveitis, but it can trigger flares in people with underlying autoimmune conditions. If your immune system is already primed to attack eye tissue, stress can act as a catalyst. Managing stress through sleep, exercise, and therapy may help reduce flare frequency - but it’s not a substitute for medical treatment.
What’s the prognosis for uveitis?
With prompt steroid treatment, most people recover full vision. Anterior uveitis has the best outlook - over 90% of cases resolve without lasting damage if treated early. Posterior and chronic forms carry higher risks, but even those can be managed with long-term monitoring and steroid-sparing drugs. The biggest risk isn’t the disease itself - it’s delay in treatment.
10 Comments
Write a comment
More Articles

Jet Lag and Time-Released Medication Dosing Across Time Zones: What Actually Works
Time-released melatonin doesn't help jet lag-it makes it worse. Learn why immediate-release melatonin, taken at the right time, is the only proven way to reset your body clock after long-haul flights.


JAY OKE
November 25, 2025 AT 16:34Been through two bouts of anterior uveitis. Steroid drops saved my vision, but man, the side effects? Cataracts by 18 months. Now I’m on methotrexate. Not fun, but better than going blind.