
Generic drugs save billions every year. In the U.S., 92% of all prescriptions filled are for generics. But behind the low price tag, a hidden risk is growing: contamination. From cancer-causing chemicals in blood pressure meds to toxic benzene in cough syrup, recent cases show this isn’t rare-it’s systemic. And the people paying the price aren’t just patients. Pharmacists, doctors, and families are caught in the fallout.
What’s Really in Your Generic Pills?
Generic drugs aren’t copies. They’re supposed to be identical in active ingredient, strength, and performance to brand-name versions. But when manufacturing goes wrong, impurities slip in. And they’re not always harmless. In 2018, the FDA found NDMA-a known human carcinogen-in valsartan, a common blood pressure drug. Levels in some batches were 200 times higher than the safe limit. That single contaminant triggered over 8,000 recalls between 2018 and 2025. By September 2025, there were 1,348 pending lawsuits from patients who developed cancer after taking contaminated valsartan. One study showed colorectal cancer rates were 7 times higher in exposed patients compared to the general population. Then came benzene. In June 2025, a lawsuit against Walgreens alleged that Mucinex, a popular expectorant, contained benzene at 4.7 parts per million. The FDA’s limit? 2 ppm. Chronic exposure above that level increases leukemia risk by 40%. Plaintiffs like Miriam Birdsong and Cheryl Mikel developed bone marrow damage after just 18 months of regular use. Oncology drugs are especially vulnerable. A STAT News investigation found 17 chemotherapy drugs from Indian manufacturers failed basic potency tests. Twelve of them had less than 80% of the labeled active ingredient. The FDA’s acceptable range is 85-115%. One hospital reported 34% treatment failure in patients given these generics-nearly triple the rate seen with verified brands. In one case, 7 out of 11 cancer patients failed to respond to treatment entirely. And then there’s fentanyl. Between 2002 and September 2025, 52 million patches were recalled due to seal failures. In one 2023 Sandoz recall, 0.8% of Duragesic patches leaked more than 15% of their dose. That’s enough to kill someone who didn’t need opioids at all.Where Is This Coming From?
The problem isn’t random. It’s concentrated. India produces 40% of the finished generic drugs sold in the U.S. and 16 of the 17 substandard cancer drugs identified in 2025 came from Indian factories. One company, Zee Laboratories, has been flagged 46 times since 2018 for quality issues-including vials filled with visible particles. China supplies 80% of the active pharmaceutical ingredients (APIs) used in U.S. generics. But the FDA inspects just 13% of Indian facilities each year. With over 28,000 foreign plants needing inspection and only $78 million in the 2025 budget for that work, that’s about 1,200 inspections total. That’s one inspection for every 23 factories. The root cause? Cost pressure. Generic manufacturers operate on razor-thin margins. A single change in a chemical process-like swapping out a solvent or adding sodium nitrite to speed up production-can introduce deadly contaminants. At ZHP, a Chinese supplier, sodium nitrite was added to valsartan production without validation. No safety checks. No testing. Just cost-cutting. And when things go wrong, records disappear. The FDA found Intas Pharmaceuticals in India shredded and burned quality documents. That’s not incompetence. That’s cover-up.Why Aren’t These Drugs Being Stopped?
The FDA doesn’t test every batch. It doesn’t even inspect every factory. It relies on manufacturers to self-report. And when they don’t? The system breaks. For years, the FDA redacted drug names in inspection reports. Even when a facility was cited for contamination, the public didn’t know which drugs were affected. ProPublica documented this practice going back to 2008. Patients couldn’t avoid risky meds. Doctors couldn’t make informed choices. In September 2025, the FDA announced a “Name Transparency Initiative” to stop hiding drug names. But it’s still early. No one knows if it’ll be enforced. The Drug Supply Chain Security Act (DSCSA) requires full electronic tracing of drugs by 2027. But right now, only 62% of pharmacies can verify where a drug came from. That means if a batch is contaminated, you might not know if your pills are part of it. And while the FDA has pushed for modern manufacturing like continuous production-which can reduce contamination by 78%-only 3% of Indian plants use it. Upgrading costs $5-15 million. For a company selling pills for pennies, that’s not worth it.
What Can You Do?
You can’t control the factory. But you can take steps to protect yourself.- Check recall lists weekly. A 2025 Pharmacy Times survey found 68% of pharmacists now check FDA recall notices every week. You should too. Go to fda.gov/drugs/drug-safety-and-availability/drug-recalls.
- Ask your pharmacist about the manufacturer. If your generic is made by Zee Laboratories or ZHP, ask if there’s a safer alternative. Many pharmacies carry multiple generic brands.
- Monitor your response. If your blood pressure suddenly spikes on valsartan, or your thyroid levels go wild on levothyroxine, it might not be your body-it’s the batch. Tell your doctor. Request a brand-name version if needed.
- Report side effects. Use the FDA’s MedWatch system. One report won’t stop a recall. But 1,000 might.
What’s Changing?
The system is finally starting to react. In April 2025, the FDA took the unusual step of punishing ZHP not just for contamination, but for destroying records. That’s a shift-from punishing bad drugs to punishing bad behavior. The new GDUFA III rules, effective June 2025, now require real-time stability testing for high-risk drugs like chemotherapy and blood pressure meds. That means manufacturers can’t wait until after shipping to check if a batch is safe. The FDA’s 2026-2030 plan includes AI tools to predict contamination risks before they happen. And blockchain tracking could one day let you scan a pill bottle and see every step of its journey-from raw chemical to pharmacy shelf. But experts like Dr. Dinesh Thakur, a former industry insider turned whistleblower, aren’t optimistic. “Without real penalties,” he says, “manufacturers will keep cutting corners. They know the cost of a recall is less than the cost of quality.”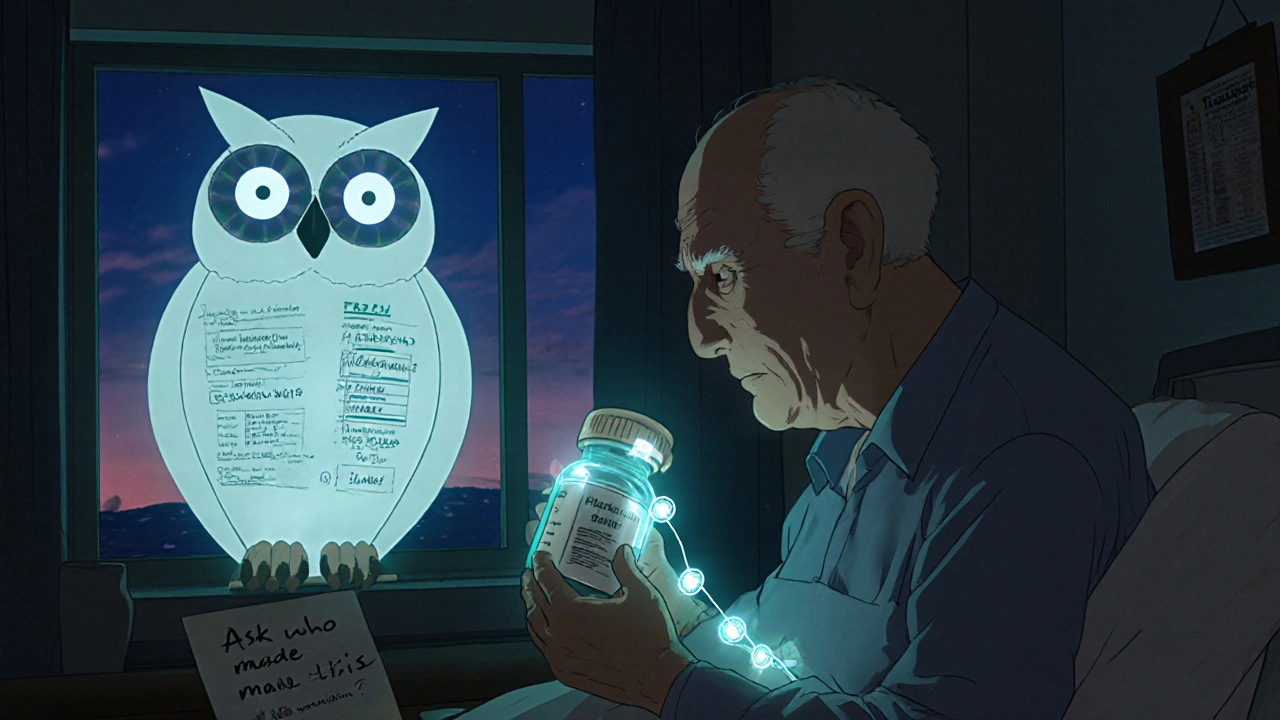
The Bottom Line
Generics are essential. They make life-saving drugs affordable. But affordability shouldn’t mean acceptability of risk. The data is clear: contamination isn’t rare. It’s predictable. And it’s escalating. Valsartan, Mucinex, chemotherapy, fentanyl patches-all these are not isolated failures. They’re symptoms of a system stretched too thin. You’re not paranoid for asking questions. You’re informed. The next time you pick up a generic prescription, don’t just take it. Ask: Who made this? Is it on a recall list? And if you’re on a life-critical drug like insulin, levothyroxine, or chemotherapy-don’t hesitate to ask for the brand name. It might cost more. But it might also save your life.Are generic drugs less safe than brand-name drugs?
Most generics are safe and effective. The FDA requires them to meet the same standards as brand-name drugs. But contamination issues have become more common in recent years, especially with foreign-manufactured generics. The problem isn’t that generics are inherently unsafe-it’s that cost pressures and weak oversight in some factories have led to dangerous lapses. The same active ingredient can be produced safely or unsafely, depending on the manufacturer.
How do I know if my generic drug has been recalled?
Check the FDA’s Drug Recalls page at fda.gov/drugs/drug-safety-and-availability/drug-recalls. You can search by drug name, manufacturer, or recall date. Many pharmacies also send out recall alerts via email or text. If you’re unsure, ask your pharmacist to verify your medication against the latest recall list. Keep your prescription bottle-it has the lot number, which is needed to confirm if your batch is affected.
Can contaminated generics cause cancer?
Yes. NDMA, found in contaminated valsartan and other ARBs, is a known human carcinogen. Studies show patients exposed to high levels had a 3.2 times higher risk of developing cancer. Colorectal cancer rates jumped from 4 per 100,000 in the general population to 27 per 100,000 in exposed patients. Benzene, found in some Mucinex products, is linked to leukemia. Long-term exposure above the FDA’s 2 ppm limit increases risk by 40%. These aren’t theoretical risks-they’ve been documented in lawsuits and medical records.
Why are so many generics made in India and China?
It’s about cost. Labor, regulatory oversight, and manufacturing infrastructure are cheaper in these countries. India produces 40% of U.S. generic finished drugs, and China makes 80% of the active ingredients. The U.S. relies on them because it’s cheaper than producing drugs domestically. But this dependence has created a supply chain that’s hard to monitor. Only 13% of Indian factories are inspected annually, even though they supply nearly half of America’s generics.
Should I stop taking my generic medication?
Don’t stop taking any prescribed medication without talking to your doctor. Abruptly stopping blood pressure, thyroid, or cancer meds can be dangerous. Instead, check if your specific drug and lot number is on a recall list. If it is, contact your pharmacy for a replacement. If you’re concerned about safety, ask your doctor if a brand-name version is an option. For critical drugs like chemotherapy or insulin, the added cost of a brand may be worth the certainty of quality.
Is the FDA doing enough to prevent contamination?
The FDA has improved oversight in recent years, but it’s still overwhelmed. With only 1,200 inspections per year for over 28,000 foreign facilities, it’s impossible to catch everything. Recent actions like banning record destruction and requiring real-time testing are steps in the right direction. But without more funding, stricter penalties, and independent audits, the system remains vulnerable. Many experts believe the FDA needs to shift from inspection to prevention-using AI and blockchain to predict and stop contamination before drugs leave the factory.
What Comes Next?
The Valsartan litigation is set to go to trial in September 2025. If courts find manufacturers knew about NDMA risks as early as 2012 and hid them, it could set a legal precedent that changes how the entire industry operates. Fines could rise. Executives could face personal liability. That’s the kind of pressure that forces real change. Until then, stay informed. Ask questions. Demand transparency. Your health isn’t a commodity. It shouldn’t be treated like one.12 Comments
Write a comment
More Articles

ACE Inhibitors and ARBs: What You Need to Know About Interactions and Cross-Reactivity
ACE inhibitors and ARBs treat high blood pressure and kidney disease but shouldn't be combined. Learn why mixing them raises risks of kidney failure and high potassium-and what safer alternatives exist.



Ashley Unknown
November 18, 2025 AT 03:50Okay but have you seen the videos? The ones where the pills are just floating in vats of murky green sludge? I saw a whistleblower leak footage from Zee Labs - they’re using tap water to rinse the pills. And the workers? They’re wearing flip-flops. I’m not even kidding. The FDA is in on it. They get kickbacks from the big pharma conglomerates. This isn’t contamination - it’s intentional poisoning. They want us sick so we keep buying more drugs. I checked my valsartan bottle - the lot number ends in 777. That’s not a coincidence. The Illuminati runs the FDA now. I’m switching to herbal tea and praying to the moon goddess. 🌙💊