Cyclosporine Level Monitor
Cyclosporine Level Checker
Check if your cyclosporine level is within safe range for your transplant stage
Result
Why This Matters
Cyclosporine toxicity can cause irreversible kidney damage. Maintaining levels within the target range reduces risk by up to 70%. Always follow your transplant team's advice for dose adjustments.
When someone gets a kidney, heart, or liver transplant, cyclosporine is often the drug that keeps their body from rejecting the new organ. But here’s the catch: cyclosporine can damage the very kidneys it’s meant to protect. This isn’t just a side effect-it’s the main reason some transplants fail. And it’s not rare. Studies show 30 to 50% of long-term kidney transplant failures are tied to how cyclosporine affects the kidneys. The good news? You can prevent most of this damage-if you know exactly how to monitor it.
Why Cyclosporine Harms the Kidneys
Cyclosporine doesn’t just sit there. It tightens the blood vessels inside the kidneys, reducing blood flow. Think of it like squeezing a garden hose-less water gets through, and the kidneys start to struggle. This isn’t just a temporary blip. Over time, it causes real structural damage: thickening of tiny arteries, changes in kidney tubules, and even scarring. The higher the drug level, the worse it gets. And unlike some side effects, this one doesn’t always show up in symptoms until it’s too late.
What makes it worse is that cyclosporine’s window for safety is razor-thin. Too little, and the body attacks the transplant. Too much, and the kidneys start shutting down. The difference between saving the organ and wrecking it can be as small as 50 ng/mL. That’s why you can’t just guess the dose. You have to measure it.
How to Measure Cyclosporine Levels
There are three main ways to measure cyclosporine in the blood: immunoassays, HPLC, and LC-MS/MS. Most labs used to rely on immunoassays-they’re fast and cheap. But they’re flawed. These tests can’t tell the difference between cyclosporine and its metabolites. And those metabolites? They’re inactive. But the test thinks they’re the real drug. So you get a reading that looks high, when it’s not. That leads to unnecessary dose cuts, which then raises the risk of rejection.
Today, the gold standard is LC-MS/MS-liquid chromatography-tandem mass spectrometry. It’s accurate to 99.2%. It doesn’t get fooled by metabolites. It can detect levels as low as 5 ng/mL. And since 2021, 92% of U.S. transplant centers have switched to it. The cost is higher, sure. But the payoff? Fewer mistakes, fewer rejected organs, and less kidney damage.
Here’s what matters: blood must be drawn at the right time. The old way was to check the trough level-just before the next dose. But research shows that’s not enough. The C2 level-two hours after the dose-is a much better predictor of how much drug the body actually absorbed. One study found C2 monitoring cut nephrotoxicity by over 22%. That’s not a small win. That’s life-changing for transplant patients.
What the Numbers Mean
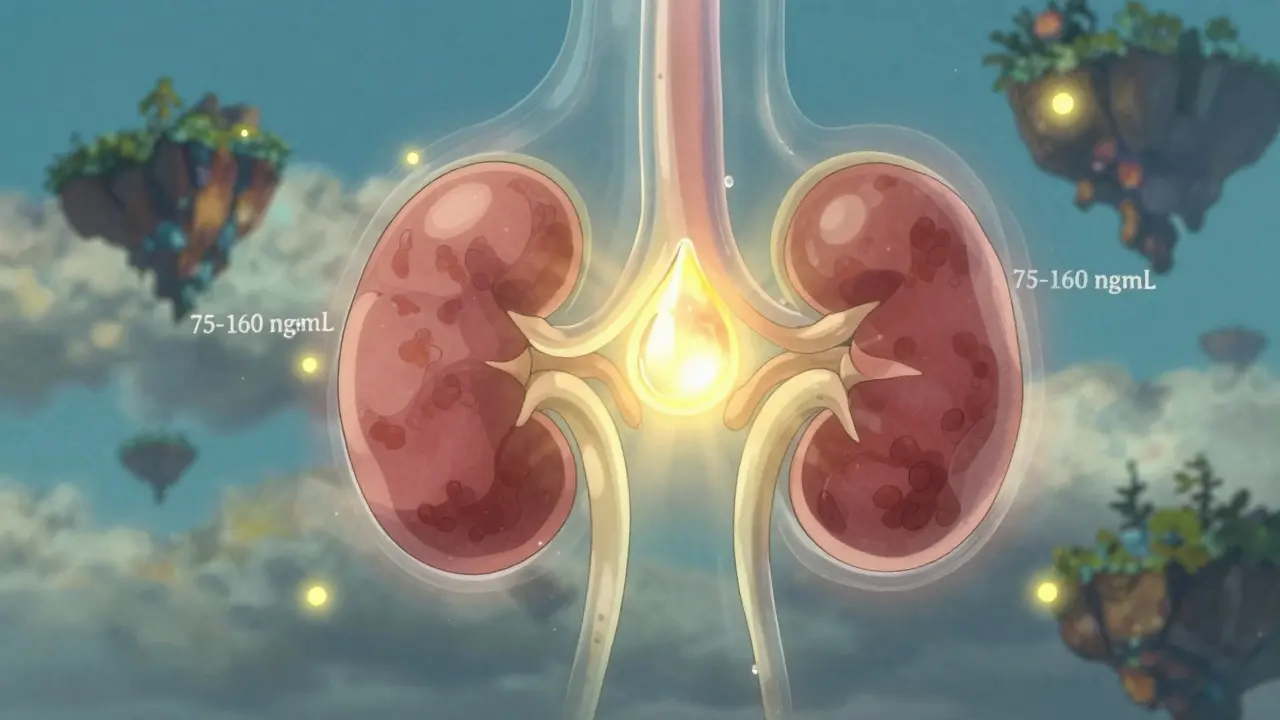
There’s no one-size-fits-all target. It depends on the organ, the time since transplant, and even your genes. For kidney transplants:
- Week 1: 200-400 ng/mL
- Week 2 to 6 months: 125-275 ng/mL
- 7 to 12 months: 100-150 ng/mL
- After 1 year: 75-160 ng/mL
For heart and liver transplants, the ranges are similar to the later stages of kidney transplants. But here’s the twist: some people metabolize cyclosporine faster than others because of their CYP3A5 gene. If you’re an extensive metabolizer, you might need 30-40% more drug just to reach the same level as someone else. That’s why personalized dosing isn’t just fancy-it’s necessary.

What Else to Monitor Alongside Cyclosporine
Looking at the drug level alone isn’t enough. You need to see how the kidneys are responding. That means checking:
- Serum creatinine-aim for under 1.5 mg/dL. A steady rise is a red flag.
- BUN-to-creatinine ratio-keep it under 20:1. Higher numbers suggest reduced kidney blood flow.
- Magnesium-cyclosporine drains magnesium. Levels below 1.7 mg/dL mean trouble.
- Blood pressure-target under 130/80 mmHg. High BP + cyclosporine = double damage.
Uric acid? It can rise, but it’s not a reliable marker. Stick to the big four. And don’t forget: cyclosporine interacts with a lot of other drugs. Ketoconazole can spike cyclosporine levels by 50%. Rifampin can crash them by 60%. Even grapefruit juice can mess with it. If a patient starts or stops another medication, check the cyclosporine level within 3-5 days.
How Often Should You Test?
Monitoring isn’t a one-time thing. It’s a rhythm.
- First month after transplant: twice a week
- Months 2-6: weekly
- Months 7-12: every two weeks
- After one year: monthly, unless something changes
And if the dose changes? Wait 4-6 weeks before checking again. Cyclosporine takes time to reach steady state. Testing too soon gives you false data. Also, use EDTA tubes-not serum tubes. Serum tubes can falsely inflate levels by 15-20%. That’s enough to send someone down the wrong path.
Can the Damage Be Reversed?
Yes. And that’s the most important thing to know. If caught early, kidney damage from cyclosporine can improve. Studies show that within three months of lowering the dose, kidney function often gets better. Blood pressure drops. Creatinine levels fall. Magnesium rebounds. The key is catching it before scarring sets in. That’s why regular monitoring isn’t bureaucracy-it’s prevention.
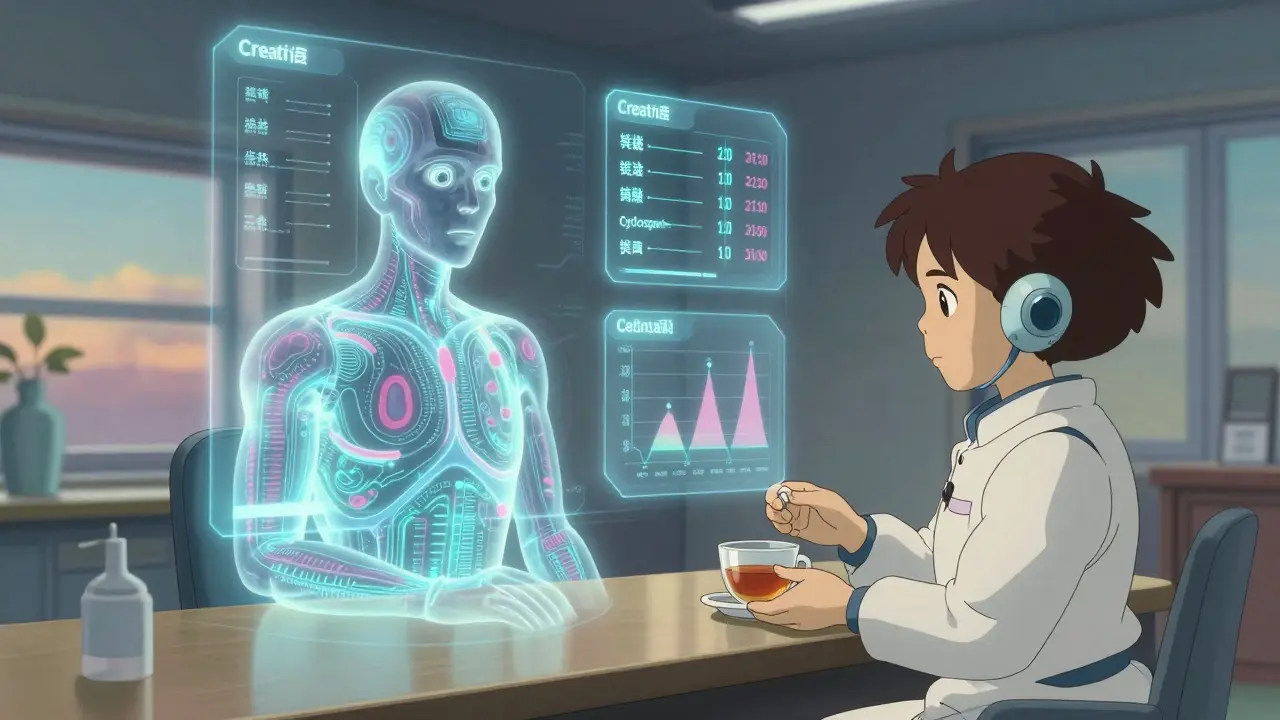
What’s Next for Monitoring?
AI is coming. Clinical trials are testing algorithms that use 17 different factors-dose, timing, genetics, diet, other meds-to predict the perfect cyclosporine dose. One model got it right 89.7% of the time. That could mean fewer blood draws and less guesswork.
Point-of-care devices are also in development. Imagine a machine in your transplant clinic that gives you a full blood level result in 15 minutes. Phase 3 trials are underway, with FDA approval expected by late 2025. That’s not science fiction. It’s the next step.
For now, the rules are simple: use LC-MS/MS, check C2 levels, monitor creatinine and magnesium, adjust for drugs and genes, and never assume. Cyclosporine is still vital. But it’s a scalpel, not a sledgehammer. Handle it right, and it saves lives. Handle it wrong, and it takes them.
Can cyclosporine nephrotoxicity be completely avoided?
No, it can’t be completely avoided, but it can be significantly reduced. With proper monitoring using LC-MS/MS, targeting C2 levels, managing drug interactions, and adjusting for genetic differences, up to 70% of severe kidney damage can be prevented. The goal isn’t zero risk-it’s minimizing risk while keeping the transplant alive.
Why is LC-MS/MS better than immunoassays for cyclosporine testing?
LC-MS/MS can distinguish between cyclosporine and its metabolites, which other tests can’t. Immunoassays often overestimate the actual drug level by 10-15%, leading to unnecessary dose reductions and higher rejection rates. LC-MS/MS has 99.2% specificity and detects levels as low as 5 ng/mL, making it the most accurate method available today.
Does everyone need C2 monitoring, or just high-risk patients?
All transplant patients on cyclosporine benefit from C2 monitoring, not just high-risk ones. Studies show C2 levels correlate more strongly with total drug exposure than trough levels. Centers using C2 monitoring report 18-22% fewer cases of nephrotoxicity. It’s now considered the standard of care in most major transplant centers.
How long does it take for kidney function to improve after lowering cyclosporine?
Improvement can begin within weeks, but significant recovery usually takes 2-3 months. Creatinine levels often drop, blood pressure improves, and magnesium levels rebound. The earlier you reduce the dose after detecting early signs of toxicity, the better the outcome. Delaying action increases the chance of permanent scarring.
Can diet or other medications affect cyclosporine levels?
Yes, significantly. Grapefruit juice, ketoconazole, and diltiazem can raise cyclosporine levels by 30-50%. Rifampin, phenytoin, and St. John’s wort can lower them by 40-60%. Even changes in fat intake can alter absorption. Any new medication or supplement should trigger a cyclosporine level check within 5 days.
More Articles
Eicosapentaenoic Acid: The Secret Ingredient for Boosting Your Overall Health and Well-being
Eicosapentaenoic Acid (EPA) has recently caught my attention as a secret ingredient that can significantly improve our overall health and well-being. Found in fish oil, this omega-3 fatty acid is known to reduce inflammation, lower the risk of heart disease, and even improve mental health. I've noticed that incorporating EPA-rich foods, like salmon and mackerel, into my diet has made a positive impact on my energy levels and mood. Additionally, taking fish oil supplements has been a convenient way to ensure I'm getting enough EPA. I highly recommend looking into EPA as a natural way to boost your health and well-being.
Sexually Transmitted Infections in the LGBTQ+ Community: Risks and Prevention Strategies
In my recent exploration on the topic of Sexually Transmitted Infections (STIs) in the LGBTQ+ community, I found that this group faces unique risks and challenges. The stigma, discrimination, and lack of understanding can often lead to higher rates of STIs. The key to combating this issue is through informed prevention strategies, which include regular testing, protected sex, and open communication about sexual health. It's crucial that we work towards creating an environment where everyone feels safe and educated about their sexual health. Remember, knowledge is power when it comes to preventing STIs.