
Dyskinesia Impact Severity Checker
This tool helps you understand how dyskinesia symptoms may affect your daily life by assessing the severity of common symptoms. Select the severity level for each listed activity to get a personalized impact score.
Morning Routine
Difficulty with basic self-care tasks like brushing teeth or getting dressed.
Work Performance
Impact on productivity, precision, or ability to complete tasks.
Social Interactions
Feelings of embarrassment or anxiety during social events.
Physical Activity
Ability to engage in regular exercise or physical movement.
Sleep Quality
Disruption due to nighttime movements or discomfort.
Daily Planning
Need to modify schedules or avoid certain activities.
Your Dyskinesia Impact Summary
Imagine trying to pour a cup of coffee while your arm suddenly jerks, or watching a favorite TV show and the characters’ faces blur as your own muscles twitch uncontrollably. That's a snapshot of life with dyskinesia impact - a challenge many people with Parkinson's disease face every day.
Quick Takeaways
- Dyskinesia are involuntary movements caused mainly by long‑term levodopa use.
- They can disrupt work, relationships, and simple tasks like dressing.
- Medication timing, deep‑brain stimulation, and tailored exercise can reduce severity.
- Support from caregivers and peer groups is essential for mental well‑being.
- Emerging wearables help track episodes and inform treatment adjustments.
What Is Dyskinesia?
Dyskinesia is a movement disorder characterized by involuntary, erratic, and often rhythmic muscle contractions. It most commonly appears in people treated for Parkinson's disease (a progressive neurodegenerative condition affecting the basal ganglia) after several years of levodopa (the primary dopamine‑replacing medication used to control Parkinson’s motor symptoms).
The brain’s dopamine pathways become hypersensitive, so when the drug’s blood level spikes, the motor circuits overreact, resulting in those unwanted movements. Types include peak‑dose dyskinesia (occurs when medication peaks), diphasic dyskinesia (appears as levels rise and fall), and off‑period dyskinesia (during low drug levels).
How Dyskinesia Shows Up in Everyday Life
Below is a personal account that mirrors many patients’ stories. I’ll walk through typical scenarios to illustrate the real‑world burden.
- Morning routine: As the first dose of levodopa hits, my hand starts twitching. Brushing teeth becomes a coordination puzzle; the toothbrush slips, and I have to pause, reset, and start again.
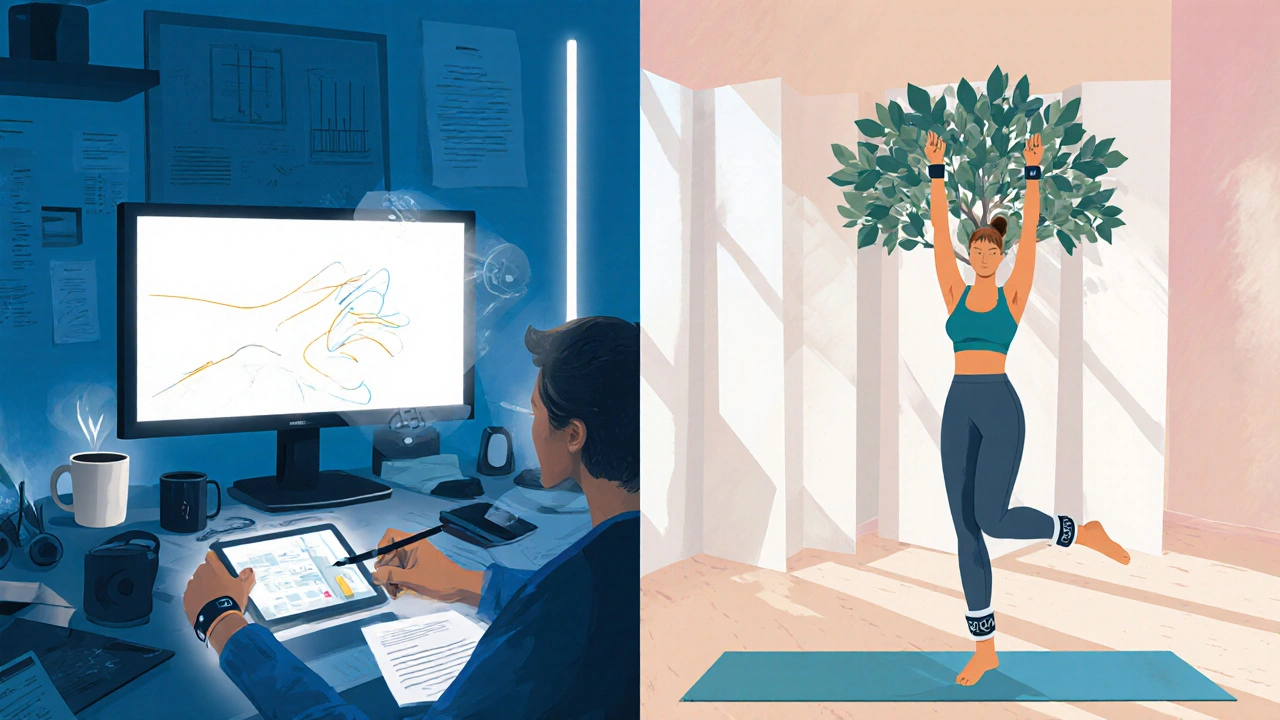
- At work: I’m a graphic designer, and my job demands steady hand movements. During peak‑dose periods, my cursor jumps, lines wobble, and deadlines scramble. I now schedule the most detail‑heavy tasks during medication “off” windows.
- Social outings: Meeting friends for dinner feels risky. A sudden foot‑tap can embarrass me, and I worry about being judged. I’ve learned to sit near the exit, just in case I need to step away.
- Physical activity: Exercise is vital, but cycling while my legs spasm can be unsafe. I’ve switched to low‑impact yoga, where controlled breathing helps smooth the movements.
- Sleep: Nighttime dyskinesia often wakes me, leaving me exhausted. A weighted blanket and a consistent bedtime routine mitigate the disruption.
These snippets reveal how dyskinesia permeates every routine, shaping decisions from clothing choices (looser fabrics) to travel plans (extra time for bathroom breaks).
Managing Symptoms: What Works and When
Effective management blends medication tweaks, surgical options, therapy, and technology. Below is a quick comparison of the most common approaches.
| Strategy | How It Helps | Typical Candidates | Key Drawbacks |
|---|---|---|---|
| Medication timing adjustment | Reduces peak‑dose spikes by splitting doses or using extended‑release forms | Early‑stage patients with fluctuating levodopa levels | May increase “off” time, requiring careful monitoring |
| Adjunctive meds (e.g., anticholinergic drugs that dampen excessive acetylcholine activity) | Dampens muscle overactivity without altering dopamine | Patients with severe tremor‑dominant dyskinesia | d>Side‑effects: dry mouth, constipation, cognitive fog|
| Deep Brain Stimulation (DBS) surgical implantation of electrodes that modulate basal‑ganglia activity | Can sharply cut dyskinesia severity and improve motor control | Advanced Parkinson’s with medication‑refractory dyskinesia | Neurosurgical risks, need for programming adjustments |
| Physical therapy & targeted exercise | Improves muscle strength, balance, and proprioception, easing involuntary movements | All stages; especially beneficial post‑DBS | Requires consistent attendance, therapist expertise |
| Wearable sensor monitoring | Tracks frequency and amplitude of movements, informing dose tweaks | Tech‑savvy patients seeking data‑driven care | Cost, data privacy concerns, variable accuracy |
Most of us blend several of these tools. For example, I switched to a controlled‑release levodopa formulation, added a low‑dose anticholinergic, and now wear a wrist‑mounted sensor that logs my tremor intensity. My neurologist reviews the data monthly, adjusting doses before symptoms flare.
The Role of Caregivers and Support Networks
Living with dyskinesia isn’t a solo journey. A caregiver (often a family member or close friend who assists with daily tasks and emotional support) can make the difference between isolation and empowerment.
My sister, for instance, learned to recognize my “off” windows and prepares low‑stimulus meals during those times. She also attends my physiotherapy sessions, helping me practice balance drills at home. Peer groups-both in‑person meet‑ups and online forums-offer practical hacks, like using weighted utensils to steady a shaking hand.
When caregivers feel overwhelmed, they risk burnout, which can indirectly worsen the patient’s condition. Encourage them to seek respite services, counseling, or local Parkinson’s support organizations.
Practical Tips to Smooth Daily Life
- Plan medication schedules meticulously. Use a pillbox with alarms; write down exact times, not just “morning”.
- Adopt ergonomic tools. Slip‑on shoes, Velcro fasteners, and weighted pens counteract tremor‑related clumsiness.
- Structure exercise routines. Warm‑up with slow stretches, then move to balance‑focused yoga or TaiChi, which have been shown to reduce dyskinesia amplitude.
- Optimize home layout. Keep pathways clear, add non‑slip mats, and install grab bars in the bathroom.
- Utilize technology. Sync wearable data to your electronic health record (EHR) if your clinic supports it. Apps like “Parkinson’s Tracker” graph dyskinesia episodes over weeks.
- Communicate with your medical team. Bring sensor logs, medication diaries, and a list of side‑effects to each appointment.
- Mind your mental health. Practice mindfulness or breathing exercises during high‑twitch periods to lower anxiety, which can amplify movements.
Small adjustments compound into a smoother day‑to‑day experience.
Looking Ahead: Research and Emerging Tools
Scientists are exploring novel therapies that could shift the treatment landscape. Gene‑editing techniques aim to boost intrinsic dopamine production, potentially eliminating the need for levodopa. Meanwhile, closed‑loop DBS systems-where sensors detect dyskinesia in real time and adjust stimulation automatically-are undergoing clinical trials with promising early results.
Wearable tech continues to evolve. The latest generation of inertial measurement units (IMUs) can differentiate between tremor, dystonia, and voluntary movement, giving clinicians a richer picture of motor fluctuations. As these devices become more affordable, they’ll likely move from research labs into everyday clinics.
For now, staying informed about these advances empowers patients to discuss options confidently with their neurologists.

Frequently Asked Questions
Why does dyskinesia appear after years of levodopa use?
Long‑term levodopa creates pulsatile dopamine spikes that overstimulate the basal ganglia’s dopamine receptors. Over time, these receptors become hypersensitive, producing involuntary movements when drug levels peak.
Can adjusting medication timing reduce dyskinesia?
Yes. Splitting the daily levodopa dose into smaller, more frequent servings or switching to extended‑release formulations smooths plasma concentration, often lessening peak‑dose dyskinesia.
Is deep‑brain stimulation safe for older adults?
DBS is generally safe for patients up to their late 70s, provided they have good overall health and no uncontrolled medical conditions. Risks include infection, lead migration, and the need for periodic device programming.
How can a caregiver help during a dyskinesia episode?
Stay calm, ensure the environment is safe (remove sharp objects), and gently guide the person to a seated position. Offering a calming distraction-like soft music-can also reduce anxiety‑driven worsening.
Are there any lifestyle changes that can lessen dyskinesia?
Regular low‑impact exercise, adequate hydration, balanced nutrition, and stress‑management techniques (meditation, breathing exercises) have all been linked to reduced severity of involuntary movements.
9 Comments
Write a comment
More Articles

Buy Cheap Generic Tetracycline Online - Safe Tips & Price Comparison
Learn how to safely buy cheap generic tetracycline online in Australia, check TGA registration, compare prices, and avoid counterfeit risks.
Pregnancy and Generics: What Safety Data Really Says for Expectant Mothers
Generic medications during pregnancy are just as safe as brand-name drugs, backed by FDA regulations and clinical data. Learn what the evidence says about active ingredients, inactive fillers, and real-world outcomes for expectant mothers.


Tiffany Owen-Ray
October 1, 2025 AT 14:12Finding balance in daily routines is a practice of mindfulness, especially when involuntary movements interrupt the flow. Scheduling medication with realistic windows can turn unpredictability into a manageable pattern. Simple ergonomic tools-like Velcro shoes or weighted pens-reduce the friction that tremor creates. Encourage a supportive environment at work by communicating your schedule so colleagues can adapt tasks during peak‑dose periods. Remember that each small adaptation compounds into a smoother day, reinforcing both physical and mental resilience.