
For most people, generic drugs are the quiet heroes of the healthcare system. They’re the affordable version of that pill your doctor prescribed - same active ingredient, same effect, but a fraction of the price. But here’s the thing: that price isn’t stable. It doesn’t just go down over time. It jumps, drops, and sometimes vanishes entirely - all within a single year.
Take lisinopril, a common blood pressure med. In early 2022, you could walk into Walmart and pay $4 for a 30-day supply. By the end of 2023, that same prescription cost $45. That’s not a typo. That’s a 247% increase in 18 months. And you didn’t get a better pill. It’s the exact same drug. The only thing that changed? The number of companies making it.
This isn’t an isolated case. Between 2013 and 2018, the price of generic nitrofurantoin - a simple antibiotic - went up by over 1,200%. Meanwhile, levothyroxine, used for thyroid conditions, dropped by 87% over the same period. How can the same class of medicine do both? The answer lies in competition, or the lack of it.
How Generic Drug Prices Work - And Why They Crash
When a brand-name drug’s patent expires, the door opens for other companies to make the same medicine. The first one to enter usually charges close to the original brand price. The second one? They undercut it a bit. The third? They slash it further. By the time five or six companies are making the same pill, the price often falls to 15% of what the brand charged.
This is why, on average, generic drugs cost 80 to 85% less than their brand-name versions. In 2022, generics made up 90% of all prescriptions filled in the U.S. - but only 23% of total drug spending. That’s how much money they save. The Congressional Budget Office estimates that between 2008 and 2017, generics saved the U.S. healthcare system $2.2 trillion.
But here’s the catch: this only works when there are enough makers. If only one or two companies produce a drug, there’s no real competition. And that’s when prices start to climb - sometimes wildly.
The Year-by-Year Roller Coaster
Looking at the data across years reveals a pattern that’s anything but smooth.
- In 2017, the FDA approved 843 new generic drugs - the most in its history. That surge pushed prices down and saved an estimated $8.8 billion that year alone.
- By 2022, the number of new approvals had slowed, and price increases began creeping back. That year, about 40 generic drugs saw list price hikes averaging 39%.
- In 2023, the overall average increase for generics was 4.9%. Sounds low? It is - until you realize that number hides extreme outliers. Around 15% of generics saw price swings over 20%, and 8.2% of prescriptions jumped between 100% and 500% in just one year.
Why does this happen? It’s not random. It’s tied to how many companies are left in the game.
Dr. Aaron Kesselheim from Harvard found that 78% of all generic price increases over 100% happened in markets with three or fewer manufacturers. When one company leaves - because of a quality issue, a shutdown, or a decision to exit a low-margin market - the remaining ones can raise prices without fear of losing customers.
Between 2013 and 2018, the number of active generic manufacturers dropped from 150 to 80. The top 10 now control 70% of the market. That’s not competition. That’s a cartel waiting to happen.

Why Some Drugs Are More Vulnerable Than Others
Not all generics are created equal. Some are easy to make. Others? Not so much.
Drugs like metformin (for diabetes) or amoxicillin (an antibiotic) are simple to produce. Thousands of companies can make them. Their prices stay low and steady.
But look at drugs like apixaban (the generic version of Eliquis) or certain heart medications. These require complex manufacturing, strict quality controls, and specialized equipment. Only a handful of factories can produce them - and many of those are overseas.
When the FDA inspected foreign generic drug plants in 2023, they found quality problems in 23% of them. When a plant fails inspection, production stops. No supply. No competition. And guess what happens to the price? It spikes.
Medicaid data from 2021 showed that 35% of generic drug shortages were linked to price increases over 50%. These aren’t accidents. They’re market failures.
What Happens When Prices Spike - And Who Gets Hurt
It’s easy to think, “Well, it’s just a generic. Who cares if it goes up a little?” But for millions of people, that “little” is life-changing.
In 2024, 37% of Medicare beneficiaries taking generic drugs said they skipped doses or cut pills in half because they couldn’t afford them. That’s nearly 4 out of 10 seniors. One woman in Ohio told her pharmacist she was taking half her levothyroxine dose because the price jumped from $12 to $60. Her doctor didn’t know. Her thyroid levels were falling. She didn’t want to be a burden.
Independent pharmacies are caught in the middle. Forty-two percent of them said they’ve had to absorb price increases on 15% of their generic inventory. Some generics flip from profitable to loss leaders in weeks. The average margin loss? $3.75 per prescription. For a small pharmacy, that’s enough to force layoffs or close shop.
And then there’s the gap between what pharmacies pay and what they get paid. The average wholesale price (AWP) listed by manufacturers is often 22% higher than what they actually pay. Medicare and Medicaid reimburse based on AWP - so when the AWP jumps, the pharmacy gets paid more. But if the real cost didn’t change, that’s a windfall for the payer, not the pharmacy. It’s a broken system.

What’s Being Done - And Why It’s Not Enough
There are efforts to fix this. The FDA’s 2024 plan includes faster reviews for generics made by only one or two companies. The FTC has 12 active investigations into unjustified price hikes. The Inflation Reduction Act removed a cap on Medicaid rebates, which pushed some brand-name drugs to lower prices - but generics barely budged.
Why? Because the law targets brand manufacturers. Generics don’t get the same rules. They’re left to the mercy of the market.
Experts like Dr. Steve Miller, former chief medical officer at Express Scripts, believe the FDA’s push for competitive generic therapies will reduce high-volatility drugs by 25% over the next five years. That’s hopeful. But it’s slow.
The real solution? More manufacturers. More factories. More transparency. Right now, we don’t even know how many companies are making most generics. The FDA doesn’t track it. The public doesn’t know. And patients are left guessing why their prescription cost suddenly doubled.
What You Can Do Right Now
If you’re paying for generics out of pocket, don’t just accept the price at the pharmacy counter.
- Use GoodRx or SingleCare. Their 2023 survey showed users saved an average of $112.50 per generic prescription - and 78% found prices at least 50% lower than what the pharmacy quoted.
- Ask your pharmacist if there’s another brand of the same drug. Sometimes, a different manufacturer’s version is cheaper, even if it’s the same active ingredient.
- If your price jumps unexpectedly, call your doctor. Ask if a different generic or alternative medication is available.
- Join patient advocacy groups. Your voice matters. When enough people report price spikes, regulators start paying attention.
Generic drugs were supposed to be the answer to high drug costs. But without real competition, they’re becoming another part of the problem. The system works beautifully when many companies are playing. When only a few are left, it breaks - and patients pay the price.
Why do generic drug prices go up even though they’re supposed to be cheaper?
Generic drug prices go up when there’s little or no competition. If only one or two companies make a drug, they can raise prices without fear of losing customers. This often happens after a manufacturer shuts down, exits the market, or faces a supply issue. The FDA found that 78% of price hikes over 100% occur in markets with three or fewer manufacturers.
Are generic drugs always the same as brand-name drugs?
Yes, by law, generic drugs must contain the same active ingredient, strength, dosage form, and route of administration as the brand-name version. They must also meet the same FDA standards for safety and effectiveness. The only differences are in inactive ingredients (like fillers or dyes) and packaging. These don’t affect how the drug works.
Which generic drugs are most likely to have price spikes?
Drugs with complex manufacturing, limited suppliers, or high demand are most vulnerable. Examples include cardiovascular drugs like amiodarone, thyroid medications like levothyroxine, antibiotics like nitrofurantoin, and newer generics like apixaban. These often have only one or two manufacturers, making them susceptible to price jumps if supply is disrupted.
How can I find the cheapest price for my generic medication?
Use free prescription savings apps like GoodRx, SingleCare, or Blink Health. These compare prices across hundreds of pharmacies and often offer coupons that cut costs by 50% or more. You can also ask your pharmacist if a different manufacturer’s version is available - sometimes the same drug from a different company costs significantly less.
Why don’t insurance plans always cover the lowest-priced generic?
Insurance plans often use a formulary that lists preferred generics, but those aren’t always the cheapest. Sometimes, the preferred drug is chosen based on rebates from manufacturers, not price. Also, some plans don’t cover all generic versions - only the ones they’ve negotiated with. Always check your plan’s formulary and ask your pharmacist if a cheaper alternative exists.
If you’re taking a generic drug and your price jumps suddenly, you’re not imagining it. The system is failing. But you’re not powerless. Know your options. Shop around. Speak up. And remember - you’re not just a patient. You’re a consumer with rights.
11 Comments
Write a comment
More Articles
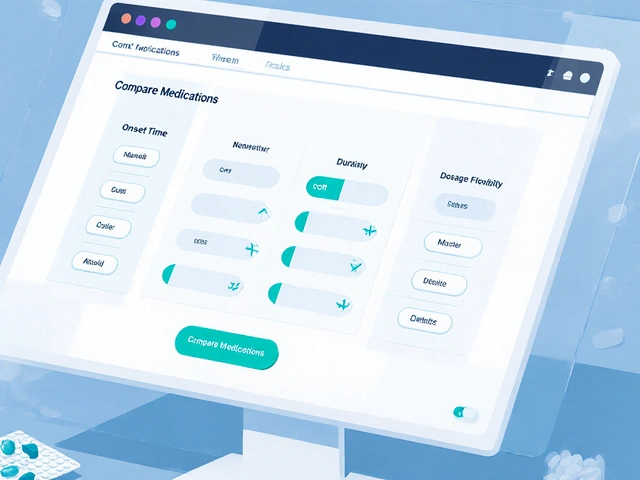
Sildamax vs Other Sildenafil Alternatives: Detailed Comparison
Compare Sildamax with other ED meds like Viagra, Cialis, Levitra, and supplements. See efficacy, cost, onset, duration, side effects, and get a decision guide.



David Palmer
December 11, 2025 AT 07:09So let me get this straight - you’re mad because pills got expensive after being cheap? Bro, everything’s a scam. I got my insulin for $5 last year, now it’s $15. Guess what? I still take it. Life goes on. Stop crying about it.