When older adults take medications, their kidneys don’t work the same way they did when they were younger. That’s not just a vague concern-it’s a real risk. About 30% of the most common drugs prescribed to seniors are cleared by the kidneys. If those kidneys aren’t working well, and dosing isn’t adjusted, toxicity can happen. A simple blood pressure pill, an antibiotic, or even a blood thinner can become dangerous. This isn’t about rare side effects. It’s about routine care that’s often done wrong.
Why Kidney Function Changes with Age
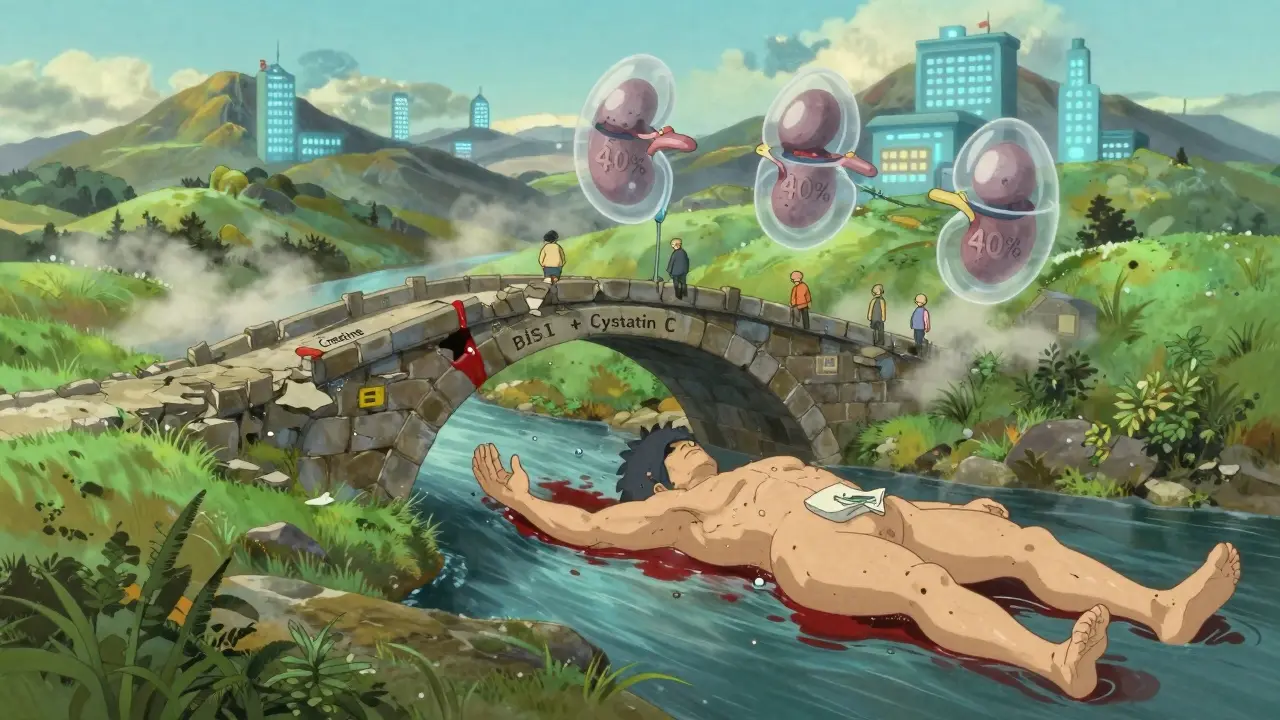
Your kidneys naturally slow down as you get older. By age 70, the average person loses about 40% of their kidney filtering capacity compared to when they were in their 20s. That’s not disease. That’s aging. The number of working filtering units (nephrons) drops. Blood flow to the kidneys decreases. Muscle mass shrinks, which changes how creatinine-a key marker doctors use-is made and cleared.
This means a “normal” creatinine level in a 75-year-old might actually mean their kidneys are barely working. If you rely on that number alone, you’ll underestimate how poorly their kidneys are functioning. And that’s when dosing errors happen.
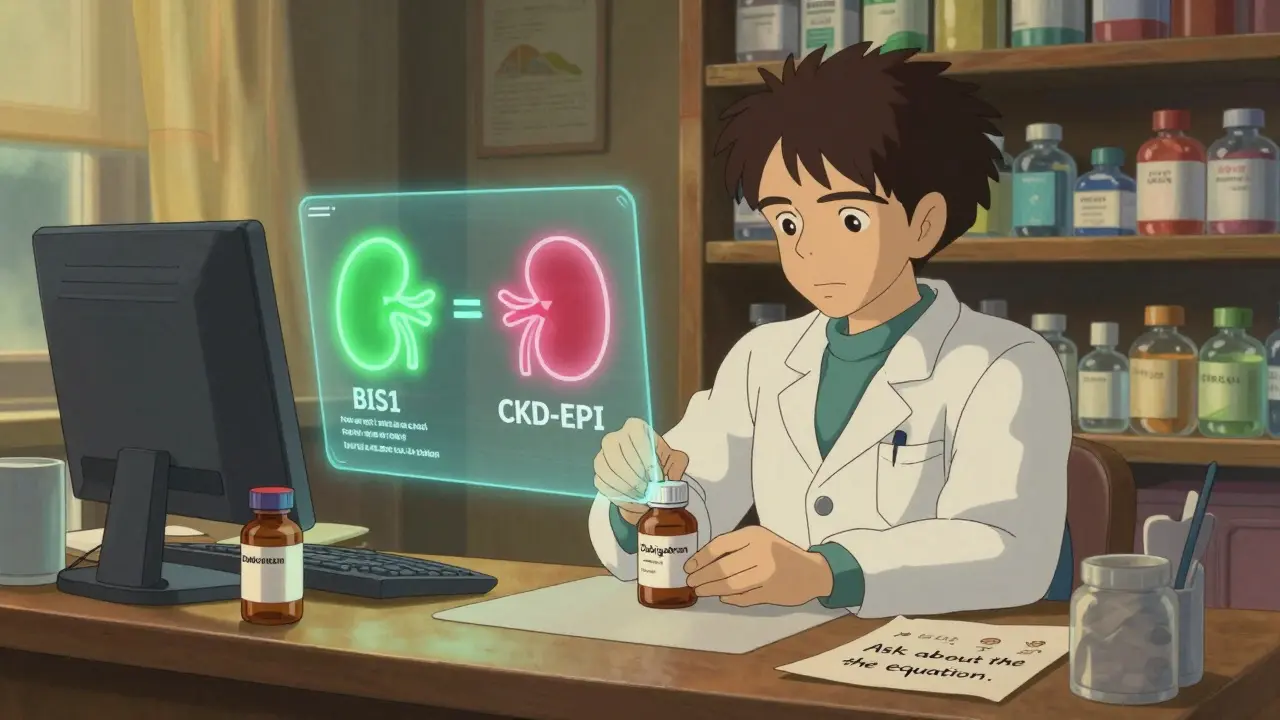
The Equations Doctors Use (and Why They’re Not All Equal)
Doctors don’t measure kidney function directly. They estimate it using equations. But not all equations are made for seniors. The most common ones are:
- Cockcroft-Gault (CG) - Developed in 1976. Uses age, weight, sex, and serum creatinine.
- MDRD - Created in 1999. Designed for people with chronic kidney disease, not healthy seniors.
- CKD-EPI - Introduced in 2009. Now the most common in electronic health records.
- BIS1 and FAS - Newer equations built specifically for older adults.
Here’s the problem: CKD-EPI and MDRD were designed for younger, sicker patients. In people over 75-especially those who are thin, frail, or have low muscle mass-these equations often overestimate kidney function by 15 to 30%. That’s not a small mistake. It’s the difference between a safe dose and a toxic one.
For example, a study of 1,200 seniors found that using the standard Cockcroft-Gault formula with actual body weight led to dosing errors in 32% of cases. But when they switched to using ideal body weight in the same formula, errors dropped to 7%. That’s a 25-point improvement just by changing one input.
Why BIS1 and FAS Are Better for Seniors
BIS1 (Berlin Initiative Study 1) and FAS (Full Age Spectrum) were developed because researchers realized older adults needed their own equations. These take into account age, sex, serum creatinine, and also factors like body composition and frailty.
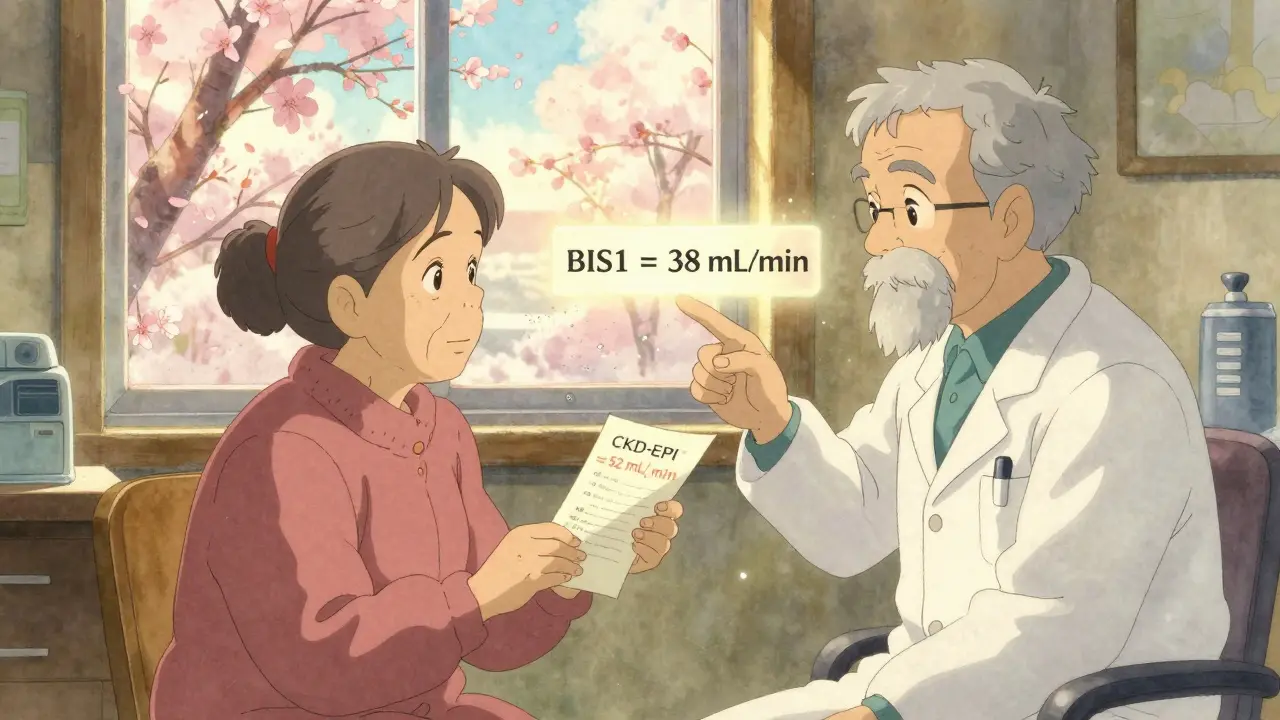
Studies show BIS1 is more accurate than CKD-EPI in people over 80. In one trial, BIS1 correctly classified kidney function in 95% of cases, while CKD-EPI got it right in only 78%. That might sound technical, but here’s what it means in practice:
- A 82-year-old woman with low muscle mass might have an eGFR of 52 mL/min using CKD-EPI.
- Using BIS1, the same person’s eGFR might be 38 mL/min.
- That changes her dosing for drugs like dabigatran or vancomycin-drugs where even a 20% overdose can cause serious harm.
Dr. Sophie Dupont’s team at the University of Michigan found that switching from CKD-EPI to BIS1 in patients over 80 reduced medication-related hospitalizations by 18%. That’s not just a number-it’s real people avoiding ER visits, falls, bleeding, or kidney failure.
When Creatinine Isn’t Enough
There’s another tool: cystatin C. Unlike creatinine, it’s not affected by muscle mass. That makes it much more reliable in seniors who are thin, bedridden, or malnourished.
But cystatin C tests cost $50-$75 more than a regular creatinine test. So it’s not done routinely. But here’s when it should be:
- Your creatinine looks normal, but you’re frail, losing weight, or have no muscle.
- Your eGFR from CKD-EPI says you’re in Stage 2 (mild decline), but you’re on a drug that needs strict dosing.
- You’ve had a recent fall or infection, and your creatinine suddenly dropped.
When cystatin C is added to creatinine, the accuracy improves. New equations like CKD2024 combine both markers and show 15% better accuracy in people over 80. This isn’t science fiction-it’s available now.
What Actually Happens in Clinics
Most electronic health records default to CKD-EPI. That’s convenient. But it’s not safe for seniors.
A 2023 survey found that 65% of primary care doctors feel unsure about which equation to use. Nearly half just go with whatever the computer picks. That’s dangerous.
Pharmacists in nursing homes report overriding EHR defaults at least once a week. One pharmacist wrote: “I’ve seen more harm from using the wrong equation than from any single drug’s side effect.”
Some hospitals are catching on. Epic Systems now automatically uses BIS1 for patients over 75. But most community clinics still rely on outdated defaults.
How to Get It Right
If you’re a senior, or caring for one, here’s how to make sure kidney function is handled correctly:
- Ask which equation was used-not just “Is my kidney function normal?” Ask: “Was it CKD-EPI, MDRD, or BIS1?”
- Check your weight and muscle status-If you’ve lost weight, are frail, or have little muscle, BIS1 or cystatin C may be needed.
- Review all medications-Drugs like warfarin, digoxin, gabapentin, and many antibiotics need adjustment. Ask your pharmacist to check each one.
- Request a cystatin C test-If your creatinine is normal but you’re at risk, this test is worth the cost.
- Use updated tools-The National Kidney Foundation’s eGFR calculator (updated 2023) and the American Geriatrics Society’s 2024 toolkit let you plug in numbers and compare equations.
The Bigger Picture
This isn’t just about dosing. It’s about how medicine treats aging. We assume “normal” lab values apply to everyone. But a 70-year-old with 40% kidney function isn’t “normal.” They’re just old.
Regulators are starting to notice. The FDA now requires drug makers to provide dosing guidance using multiple equations for older adults. Medicare is penalizing hospitals for medication errors in seniors. These are real consequences.
But change is slow. The best defense is knowledge. If you’re taking more than three medications, ask your doctor: “Which kidney function equation was used to calculate my dose? Is it the right one for me?”
There’s no magic test. No single equation works for everyone. But the right choice can mean the difference between staying healthy and ending up in the hospital.
What’s the best equation for estimating kidney function in seniors over 75?
For seniors over 75, especially those who are frail, thin, or have low muscle mass, the BIS1 or FAS equations are more accurate than CKD-EPI or MDRD. Studies show BIS1 reduces dosing errors by up to 25% in this group. While CKD-EPI is still the default in most electronic health records, geriatric specialists recommend BIS1 for patients over 75 because it accounts for age-related changes in body composition that older equations ignore.
Why is creatinine not reliable for older adults?
Creatinine is a waste product from muscle breakdown. As people age, they lose muscle mass-even if they don’t lose weight. This means less creatinine is produced, so blood levels can look normal even when kidney function is low. As a result, creatinine-based equations like CKD-EPI often overestimate kidney function in seniors by 15-30%, leading to unsafe medication doses.
Should I get a cystatin C test?
Yes, if you’re over 70, have low muscle mass, are losing weight, or are on medications that require precise dosing (like blood thinners or antibiotics). Cystatin C isn’t affected by muscle loss, so it gives a clearer picture of kidney function. It costs $50-$75 more than a creatinine test, but it can prevent dangerous overdoses. Ask your doctor if it’s right for you.
Do all pharmacies and doctors use the same method?
No. Most electronic health records automatically use CKD-EPI, even for seniors. But many pharmacists and geriatric specialists override this. A 2023 survey found 63% of pharmacists in senior care settings manually change the equation at least once a week to match the patient’s real condition. Academic centers are more likely to use BIS1, but community clinics often stick with defaults-putting patients at risk.
Can I calculate my own kidney function?
Yes, using free, updated tools. The National Kidney Foundation’s online eGFR calculator (updated November 2023) lets you enter your age, sex, race, serum creatinine, and weight, then compares results from multiple equations. You can also use the American Geriatrics Society’s 2024 clinical toolkit. Bring the results to your doctor to discuss whether your current dosing is appropriate.
Next Steps for Seniors and Caregivers
If you’re managing medications for yourself or someone else:
- Keep a list of all medications and dosages.
- Ask for the latest creatinine and eGFR results at every visit.
- Request BIS1 or cystatin C if there’s any doubt about kidney function.
- Don’t assume “normal” lab results mean safe dosing.
- Use the National Kidney Foundation’s calculator to compare results before your next appointment.
Medication safety in older adults isn’t about doing more tests. It’s about doing the right test. And that starts with asking the right question.
14 Comments
Write a comment
More Articles

Generic Immunosuppressive Combinations for Transplant Patients: Cost-Saving Options That Work
Generic immunosuppressive combinations now make lifelong transplant care affordable without sacrificing safety. Learn how tacrolimus, MMF, and sirolimus generics work, their real cost savings, and why careful monitoring is essential.

Top 7 Alternatives to Finasteride in 2025: What's Right for You?
Exploring the top alternatives to Finasteride in 2025 offers insights for those seeking different solutions for conditions like BPH and hair loss. With options like Tadalafil providing specific benefits and drawbacks, understanding how each treatment works can help guide personal health decisions. This article presents detailed comparisons to assist in finding the most suitable choice. Whether managing urinary symptoms or tackling hair loss, these alternatives offer varied paths to explore. Dive into the pros and cons to discover the best fit for your needs.

Tony Shuman
February 15, 2026 AT 20:45This is why America's healthcare system is broken. They use algorithms designed for 30-year-olds on 80-year-olds and call it 'evidence-based.' Meanwhile, real doctors who actually talk to patients are ignored. I've seen grandmas on blood thinners almost die because some EHR defaulted to CKD-EPI. No wonder people don't trust medicine anymore.