Uveitis: Causes, Treatments, and What You Need to Know
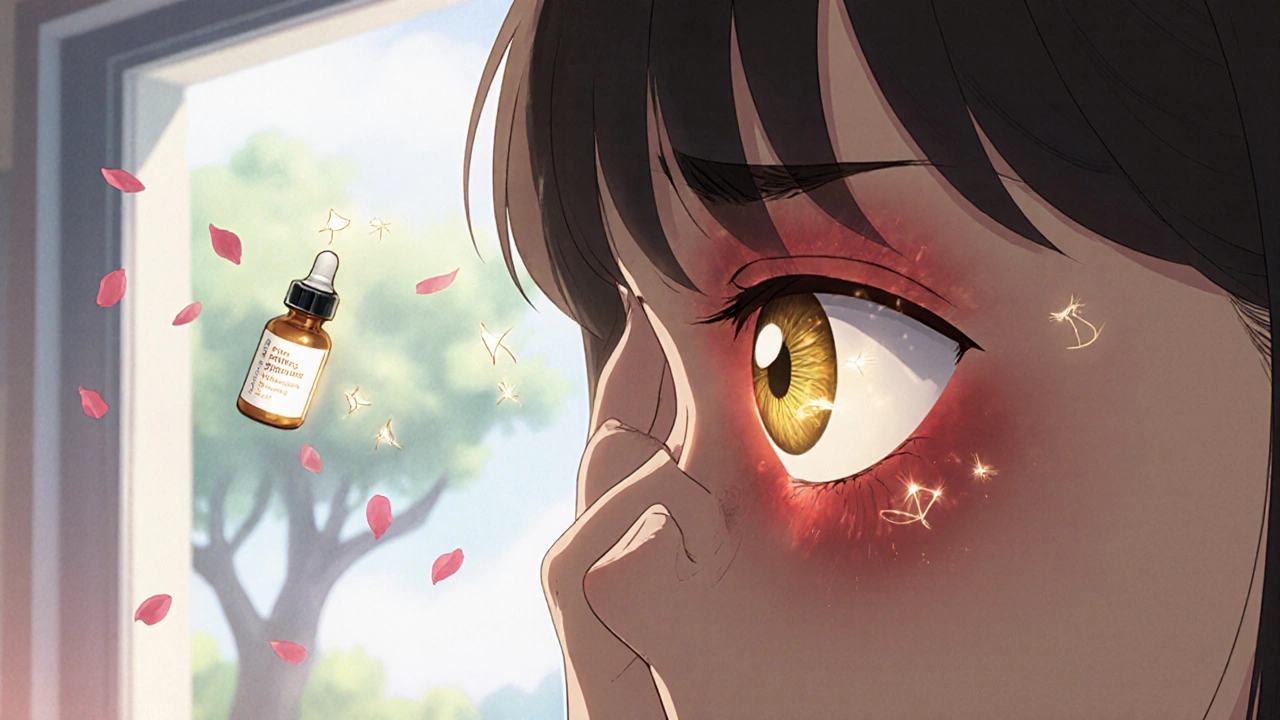
When your eye becomes red, painful, and blurry out of nowhere, it might not just be allergies or fatigue — it could be uveitis, an inflammation of the uvea, the middle layer of the eye that includes the iris, ciliary body, and choroid. Also known as intermediate or posterior uveitis, depending on where the swelling happens, this condition doesn’t always come with obvious warning signs — but it can lead to permanent vision loss if ignored. Unlike a simple eye infection, uveitis often points to something deeper: an autoimmune disorder, an infection like Lyme disease or herpes, or even a reaction to certain medications. It’s not rare — nearly 15% of blindness cases in developed countries trace back to untreated uveitis.
What makes uveitis tricky is how it hides. Some people feel a dull ache behind the eye; others see floaters or light sensitivity so severe they can’t drive at night. The inflammation can hit one eye or both, and it can flare up suddenly or creep in slowly. corticosteroid eye drops, the most common first-line treatment, reduce swelling and prevent scarring — but they’re not a cure. If the cause is an autoimmune disease like rheumatoid arthritis or ankylosing spondylitis, you’ll need to treat the root problem, not just the eye. That’s where autoimmune eye disease, a category of conditions where the immune system mistakenly attacks eye tissue comes in. Doctors now use blood tests, imaging, and sometimes even biopsies to find out if your uveitis is linked to something like sarcoidosis or multiple sclerosis.
There’s no one-size-fits-all fix. For some, a few weeks of steroid drops clears everything up. For others, oral steroids, injections around the eye, or even immunosuppressants become necessary. Newer biologic drugs are helping people who don’t respond to traditional treatments. And while uveitis can come back, early diagnosis and consistent follow-ups cut the risk of complications like glaucoma, cataracts, or retinal damage dramatically.
The posts below cover everything you won’t find in a quick Google search — from how certain medications can trigger uveitis-like reactions, to what to do when standard treatments fail, and how managing other chronic conditions like Crohn’s disease or gout can impact your eye health. You’ll get real advice on spotting warning signs early, understanding test results, and working with your doctor to avoid long-term damage. This isn’t just about eye drops — it’s about protecting your vision before it’s too late.
Uveitis: Understanding Eye Inflammation and Steroid Treatment
Uveitis is a serious eye inflammation that can lead to vision loss if untreated. Learn the signs, causes, and why steroid therapy is the critical first step to saving your sight.