
Every year, thousands of people in the U.S. end up in the hospital or worse because of a simple mistake: someone didn’t know what medicines they were taking. It’s not always a doctor’s error. Often, it’s because the patient’s medication list was outdated, incomplete, or never written down at all. The truth is, if you’re taking more than one medication-prescription, over-the-counter, vitamins, or even herbal supplements-you need a clear, current list. Not just for emergencies. For every doctor visit, every pharmacy trip, every change in your health.
Why Your Medication List Matters More Than You Think
Medication errors are one of the leading causes of preventable harm in healthcare. The FDA estimates about 7,000 deaths each year in the U.S. come from these mistakes. And most of them happen because someone didn’t have the right information at the right time. A 2020 study found that having an accurate medication list could stop 50 to 80% of errors during hospital transfers or doctor visits. That’s not a small number. That’s life or death.
Think about it: you might be seeing three different specialists. One prescribes a new blood pressure pill. Another adds a painkiller. Your pharmacist fills a refill for your cholesterol med. But none of them talk to each other. If your list isn’t updated, someone could accidentally give you a drug that reacts badly with another. Or worse-they might give you a drug you’re allergic to because no one knew you stopped taking it six months ago.
Dr. Scott Gottlieb, former FDA Commissioner, put it plainly: “Accurate medication lists are the single most important tool for preventing adverse drug events in polypharmacy patients.” That’s not just advice. It’s a safety rule backed by data.
What to Include on Your Medication List
A good medication list isn’t just a scribble on a napkin. It needs details. Here’s what to write down for every medicine you take:
- Drug name-both brand and generic (e.g., “Lipitor” and “atorvastatin”)
- Strength and dose-how much you take (e.g., “10 mg”)
- Frequency-how often (e.g., “once daily,” “every 8 hours”)
- Route-how you take it (e.g., “by mouth,” “inhaler,” “patch”)
- Purpose-why you’re taking it (e.g., “for high blood pressure,” “for occasional headaches”)
- Time of last dose-especially useful if you’re in the ER or changing providers
- Prescribing provider-who wrote the prescription (e.g., “Dr. Lee, Cardiology”)
Don’t forget the extras: over-the-counter pain relievers like ibuprofen, antacids, sleep aids, vitamins, fish oil, turmeric supplements, or herbal teas. Many people don’t think these count. But they do. A 2010 American Heart Association report found that “many people won’t mention a drug they take because it’s not prescription”-and that’s exactly where mistakes happen.
Also list any allergies and what happened when you took them. “Allergic to penicillin-rash” isn’t enough. Write “anaphylaxis-swelling, trouble breathing.” Details save lives.
Choose Your Format: Paper, App, or EHR
You have options. But not all are created equal.
Paper Lists
The FDA’s free “My Medicines” template is a solid starting point. It’s printable, simple, and doesn’t need batteries. Many hospitals still use paper forms because they’re reliable in emergencies. But here’s the catch: a 2022 study in JAMA Internal Medicine found that 43% of paper lists were outdated. That means nearly half the time, the information you’re handing your doctor is wrong.
Tip: Keep your paper list in your wallet or purse. Make a copy for your emergency contact. Update it every time you change a dose or stop a drug.
Smartphone Apps
Apps like Medisafe, MyTherapy, and CareZone let you scan pill bottles, set reminders, and even share your list with family or doctors. Medisafe has over 6 million users, and users report a 28% drop in missed doses thanks to alerts. But adoption is low among older adults. Pew Research found only 35% of people over 65 regularly use these apps. If you’re not tech-savvy, or your eyesight isn’t what it used to be, the interface can feel overwhelming.
Look for apps with large text, voice input, and simple navigation. Some let you take a photo of your pill bottle and auto-fill the details. That’s a game-changer.
Electronic Health Record (EHR) Portals
If you’re part of a large health system like Kaiser Permanente or use Epic’s MyChart, you might already have a digital list built into your patient portal. These lists sync with your doctors’ records, so changes show up in real time. A 2022 internal Epic study showed their reconciliation tools cut documentation time by 37%. But here’s the problem: only 62% of U.S. hospitals have full reconciliation workflows, and only 58% of primary care practices do. If your doctor’s office doesn’t use it, your portal list might be useless.
Best practice: Use your EHR list as a backup, not your only source. Always carry a printed version or a phone screenshot.
How to Keep It Updated-Without Forgetting
The biggest problem? Keeping it current. A University of Michigan study found that 68% of patients don’t update their list after leaving the hospital. That’s terrifying. You get a new prescription. You stop an old one. You forget to tell anyone. And suddenly, your list is a time bomb.
Here’s how to fix that:
- Update after every change-new script, canceled pill, added supplement. Do it the same day.
- Use a trigger-link list updates to something you already do. Every Sunday, when you organize your pill box, update your list. Every time you refill a prescription, check your list.
- Use the brown bag method-once a year, or before a major appointment, dump all your meds into a brown bag and bring them to your doctor. They’ll check what’s there against your list. This catches hidden supplements, expired pills, or duplicates you didn’t know you had.
- Take a photo-snap a picture of each pill bottle with your phone. Store them in a folder labeled “Medications.” If you’re ever unsure what you’re taking, pull up the photo. Geriatric pharmacists say 82% of seniors find this helpful.
- Sync renewals-ask your doctor to prescribe 90-day supplies for chronic meds (like blood pressure or diabetes drugs). That means fewer refills, fewer chances to forget a change, and less clutter on your list.
Who Should See Your List
You’re not just doing this for yourself. You’re doing it for the people who care for you.
- Your primary care doctor-review it at least once a year. More often if you’re on five or more meds.
- Pharmacists-they’re trained to catch interactions. Many Medicare Part D plans offer free Medication Therapy Management (MTM) sessions. Use them.
- Emergency responders-keep a printed copy in your wallet. Some people even wear a medical ID bracelet with a QR code linking to their list.
- A trusted family member-give them a copy. If you’re unconscious, they can tell the ER team what you’re taking.
Don’t assume your doctor “knows” your meds. They don’t. Even if you’ve been with them for years. People forget. Systems glitch. Paper gets lost. Your list is your safety net.

Real Stories, Real Risks
One Reddit user, u/NurseJenNYC, said she caught three potentially fatal drug interactions in one month just by verifying patients’ lists. Another, u/RetiredDoc1987, said he sees elderly patients with lists unchanged for two years. “They’re taking meds they stopped. Missing ones they need. It’s a disaster waiting to happen.”
Kaiser Permanente saw a 22% drop in medication-related readmissions after rolling out structured list protocols across 40 hospitals. That’s thousands of avoided hospital stays.
But the ECRI Institute documented a case where a patient died from a warfarin interaction-because the ER team relied on an outdated list. The patient had switched to a new blood thinner six weeks earlier. No one knew.
These aren’t hypotheticals. They’re happening right now.
What’s Changing in 2026
The rules are getting stricter. The Joint Commission’s National Patient Safety Goal 02.02.01 (updated January 2023) now requires medication reconciliation at every transition of care-admission, discharge, transfer, clinic visit. Hospitals that don’t comply risk penalties.
AI is stepping in. Google Health’s pilot with Mayo Clinic used voice recognition to build medication lists from patient conversations-with 89% accuracy. That’s not science fiction. It’s coming to your doctor’s office soon.
But technology won’t fix this alone. The biggest barrier? Fragmented systems. Only 37% of U.S. providers can see your full medication history across all settings. That means your list still matters more than ever.
Start Today. Don’t Wait.
You don’t need a fancy app. You don’t need to be tech-savvy. You just need to start.
Right now, grab a piece of paper. Write down every pill, capsule, patch, or drop you take. Include the name, dose, how often, and why. Add your allergies. Then, call your pharmacist or doctor and ask: “Is this list complete?”
Update it this week. Keep it with you. Share it with someone you trust. That’s not just good advice. It’s how you protect your life.
Medication safety isn’t about fancy tools. It’s about one simple habit: knowing what’s in your body-and making sure everyone else knows too.
13 Comments
Write a comment
More Articles
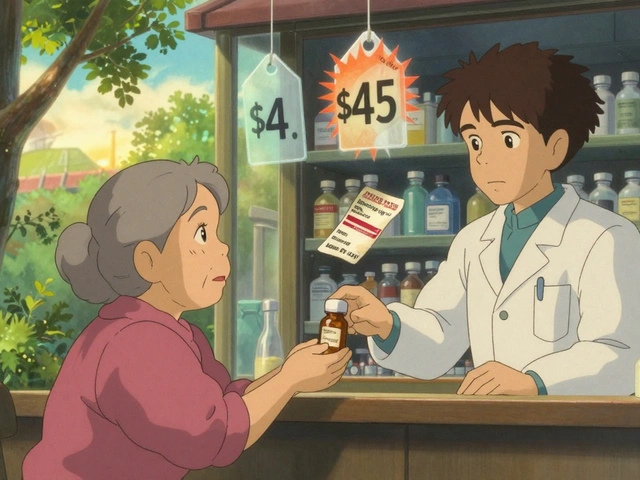
Generic Drug Prices Over Time: Year-by-Year Changes and What Really Happens
Generic drug prices don't just drop over time - they spike unpredictably. See how competition, manufacturer exits, and supply chain issues cause year-by-year price swings that impact millions of Americans.

Palliative Care in Cancer: How to Control Pain and Improve Quality of Life
Cancer pain doesn't have to be unbearable. With the right approach, 80-90% of it can be controlled. Learn how pain assessment, medications, radiation, and palliative care teams work together to restore quality of life.
Future Practice Trends: How Healthcare Provider Attitudes Are Changing by 2025
By 2025, healthcare providers are shifting from traditional roles to data-savvy partners in care. Learn how AI, patient-generated data, workforce certification, and human-centered design are reshaping provider attitudes and what it means for the future of healthcare.

Clint Moser
January 4, 2026 AT 03:02so uhm like i was reading this and it made me think-what if the whole med list thing is just a distraction? i mean, the fda’s been pushing this for years but did you know that 78% of hospital med errors happen because the ehr system auto-populates the wrong drug from a dropdown? they don’t even look at your paper list. it’s all algorithmic hallucinations now. they call it ‘reconciliation’ but it’s just data spaghetti with a badge.